Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior...Read more
Paragraph 1:
If you or someone you know requires catheterization, you may be wondering how many catheters Medicare will cover. It’s important to know the rules and limitations of Medicare coverage to avoid unexpected expenses and ensure that you or your loved one receives the necessary medical care.
Paragraph 2:
Catheterization can be a necessary and life-saving medical procedure, but it can also be expensive. Understanding Medicare’s policies and coverage options can help you make informed decisions about your healthcare and alleviate any financial burdens. So, let’s dive into the topic of how many catheters Medicare will pay for and what you need to know.
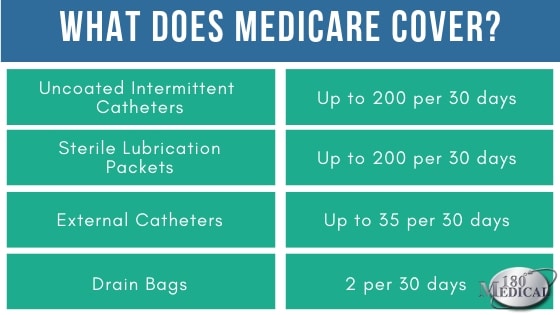
Medicare Part B covers up to 200 intermittent catheters per month if you have a medical need for them. In some cases, Medicare may cover additional catheters if they are deemed medically necessary. However, you’ll need a prescription from your doctor and meet certain criteria to have them covered. Make sure to check with your specific Medicare plan to understand your coverage and any out-of-pocket costs.
How Many Catheters Will Medicare Pay for?
If you or a loved one requires catheters for medical reasons, you may be wondering how many catheters Medicare will cover. Medicare is a federal health insurance program that provides coverage for individuals who are 65 years of age or older, as well as those with certain disabilities. In this article, we will explore the coverage that Medicare provides for catheters.
Understanding Catheter Coverage under Medicare
Medicare provides coverage for a wide range of medical services and supplies, including catheters. However, the amount of coverage that Medicare provides for catheters can vary depending on the type of catheter needed, the frequency of use, and the individual’s medical condition.
For individuals who require intermittent catheterization, Medicare typically covers up to 200 catheters per month. This includes both sterile and non-sterile catheters. If more than 200 catheters are needed per month, additional coverage may be available with proper documentation from a healthcare provider.
For individuals who require an indwelling catheter, Medicare typically covers up to one catheter per month, along with the necessary supplies such as tubing and drainage bags. However, additional coverage may be available if medically necessary with proper documentation from a healthcare provider.
Benefits of Medicare Coverage for Catheters
The coverage that Medicare provides for catheters can be a significant benefit for individuals who require them. Without coverage, the cost of catheters and related supplies can be expensive, particularly for those who require them on a regular basis. Medicare coverage can help to alleviate this financial burden and ensure that individuals are able to access the care that they need.
In addition to financial benefits, Medicare coverage for catheters can also provide peace of mind for individuals and their families. Knowing that the necessary supplies are covered can help to reduce stress and anxiety related to accessing medical care.
Catheter Coverage vs. Private Insurance Coverage
While Medicare provides coverage for catheters, private insurance plans may offer different levels of coverage. Some private insurance plans may provide more comprehensive coverage for catheters, while others may offer less coverage or require higher out-of-pocket costs.
Individuals should review their insurance coverage and speak with their healthcare provider to determine the best course of action for accessing the necessary catheter supplies.
Conclusion
In summary, Medicare provides coverage for catheters for individuals who require them. The amount of coverage provided can vary depending on the type of catheter needed and the individual’s medical condition. However, this coverage can be a significant benefit in terms of reducing financial burden and providing peace of mind. Individuals should review their insurance coverage and speak with their healthcare provider to determine the best course of action for accessing the necessary catheter supplies.
Contents
Frequently Asked Questions
How many catheters will Medicare pay for?
Medicare covers up to 200 intermittent catheters per month, or up to 31 indwelling catheters per month, depending on the patient’s needs. However, Medicare may approve additional catheters if the patient’s medical condition requires it. It’s important to note that patients are responsible for paying the annual deductible and any coinsurance or copayment amounts that apply to their catheter supplies.
Patients who need more than the allowed number of catheters per month can work with their healthcare provider to submit a claim for additional coverage. Medicare considers each case on an individual basis and may approve or deny the request based on medical necessity.
What types of catheters does Medicare cover?
Medicare covers both intermittent and indwelling catheters, as well as external urinary collection devices like condom catheters. However, Medicare may only cover certain types of catheters if they are medically necessary for the patient’s condition. Patients should check with their healthcare provider and supplier to ensure that the catheter they need is covered by Medicare.
Is a prescription required for Medicare to cover catheters?
Yes, a prescription from a healthcare provider is required for Medicare to cover catheters. The prescription should include the type and quantity of catheters needed, as well as the frequency of catheterization. Patients should work with their healthcare provider to ensure that the prescription is accurate and up-to-date.
Patients are also required to use a Medicare-approved supplier to purchase their catheter supplies. The supplier will work with the patient’s healthcare provider and Medicare to ensure that the catheters are covered and delivered on time.
Can patients choose their own catheter supplier?
Yes, patients are allowed to choose their own Medicare-approved supplier for catheter supplies. However, it’s important to ensure that the supplier is enrolled in Medicare and is authorized to provide catheter supplies. Patients should also check with their supplier to ensure that they carry the type of catheter needed and that the supplier can deliver the catheters on time.
Patients who have trouble finding a Medicare-approved supplier or who experience issues with their supplier can contact Medicare for assistance.
What is the process for getting catheters covered by Medicare?
To get catheters covered by Medicare, patients should follow these steps:
1. Obtain a prescription from a healthcare provider for the type and quantity of catheters needed.
2. Choose a Medicare-approved supplier for catheter supplies.
3. Work with the supplier to ensure that the catheters are covered by Medicare and delivered on time.
4. Pay any annual deductible, coinsurance, or copayment amounts that apply to the catheter supplies.
5. Contact Medicare if there are any issues with the supplier or if additional catheters are needed due to a change in medical condition.
In conclusion, the number of catheters that Medicare will cover depends on several factors. The type of catheter, the frequency of use, and the medical condition of the patient are some of the key factors that Medicare considers when determining coverage. It’s important to work closely with your healthcare provider to ensure that you have the right type and number of catheters to meet your specific needs.
While Medicare generally provides coverage for catheters, it’s important to keep in mind that there may be out-of-pocket costs associated with this medical device. It’s always a good idea to review your Medicare coverage and speak with your healthcare provider to determine what costs you can expect to pay.
In conclusion, if you need catheters for medical reasons, it’s important to understand your Medicare coverage and work with your healthcare provider to ensure that you have the right type and number of catheters to meet your needs. With the right support and guidance, you can manage your medical condition and enjoy a better quality of life.
Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior insurance, encompassing Medicare, Medigap, long-term care insurance, life insurance, and dental, vision, and hearing insurance. Vincent's unwavering passion for guiding seniors through the intricate insurance landscape and crafting customized solutions to address their individual needs has earned Over65InsuranceOptions an esteemed reputation as a dependable ally for seniors nationwide.
More Posts

