Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior...Read more
As we age, we may require various medical supplies to maintain our health and quality of life. One such supply is catheters, which are commonly used by individuals with urinary or bladder issues. However, many people wonder if their Medicare coverage will extend to catheter supplies. In this article, we will explore the answer to this question and provide valuable information for those in need of catheter supplies.
Medicare is a vital resource for many seniors and individuals with disabilities, providing coverage for various medical services and supplies. However, navigating the complex world of Medicare coverage can be daunting, especially when it comes to specialized supplies such as catheters. If you or a loved one require catheter supplies, it’s important to understand what is covered by Medicare to ensure you have access to the care you need.
Does Medicare Cover Catheter Supplies?
If you require catheter supplies for medical reasons, you may be wondering if Medicare covers these expenses. The answer is yes, but there are certain guidelines you need to follow to ensure you receive coverage. In this article, we will discuss what catheter supplies are, how Medicare covers them, and the requirements for receiving coverage.
What are Catheter Supplies?
Catheter supplies are medical devices used to assist with urinary incontinence or bladder retention. They come in different types, including intermittent catheters, external catheters, and indwelling catheters. Intermittent catheters are disposable or reusable and are inserted into the bladder via the urethra to drain urine, while external catheters are worn over the penis to collect urine. Indwelling catheters are inserted into the bladder and remain in place for an extended period.
Medicare Coverage for Catheter Supplies
Medicare Part B covers catheter supplies, except for external catheters, which are covered under Medicare Part D. To qualify for coverage, you must have a medical need for catheterization due to a medical condition such as prostate cancer, urinary incontinence, or a spinal cord injury. Your doctor must also prescribe the catheter supplies, and the supplier must be enrolled in Medicare.
Types of Catheter Supplies Covered by Medicare
Medicare covers several types of catheter supplies, including intermittent catheters, indwelling catheters, and disposable urinary collection devices. However, Medicare does not cover external catheters, which are covered under Medicare Part D. Additionally, Medicare may limit the number of catheter supplies you can receive per month, depending on your medical condition.
Requirements for Receiving Medicare Coverage for Catheter Supplies
To receive Medicare coverage for catheter supplies, you must have a medical need for catheterization due to a medical condition, and your doctor must prescribe the supplies. You also need to purchase the supplies from a supplier that is enrolled in Medicare. If you purchase supplies from a non-enrolled supplier, Medicare will not cover the cost.
Benefits of Medicare Coverage for Catheter Supplies
The benefits of Medicare coverage for catheter supplies are significant. You can receive high-quality catheter supplies at a reduced cost, which can save you money in the long run. Additionally, Medicare may limit the number of catheter supplies you can receive per month, which can help you manage your medical condition more effectively.
Medicare Coverage vs. Private Insurance
If you have private insurance, you may wonder if your plan covers catheter supplies. Private insurance plans may cover catheter supplies, but the coverage may vary depending on your specific plan. Additionally, you may have to pay a higher out-of-pocket cost compared to Medicare coverage.
Conclusion
In conclusion, Medicare covers catheter supplies for those who have a medical need for catheterization due to a medical condition. To receive coverage, you must have a prescription from your doctor, and you must purchase the supplies from a supplier enrolled in Medicare. Medicare coverage for catheter supplies can save you money and help you manage your medical condition more effectively.
Contents
Frequently Asked Questions
Does Medicare Cover Catheter Supplies?
Yes, Medicare covers catheter supplies for beneficiaries who meet certain conditions. Catheter supplies are considered durable medical equipment (DME) and are covered under Part B of Medicare. This includes intermittent catheters, indwelling catheters, external catheters, and sterile catheters.
To be eligible for coverage, the catheter supplies must be prescribed by a healthcare provider and deemed medically necessary. Additionally, the supplier of the catheter supplies must be enrolled in Medicare and must accept Medicare assignment, which means they agree to accept the Medicare-approved amount as payment in full.
What Types of Catheter Supplies are Covered by Medicare?
Medicare covers a variety of catheter supplies, including intermittent catheters, indwelling catheters, external catheters, and sterile catheters. The specific type of catheter supplies that are covered will depend on the individual’s medical needs and the recommendation of their healthcare provider.
It is important to note that Medicare only covers catheter supplies that are deemed medically necessary. If an individual chooses to use a catheter supply that is not covered by Medicare, they will be responsible for the full cost of the supplies.
How Much Does Medicare Cover for Catheter Supplies?
Medicare covers 80% of the Medicare-approved amount for catheter supplies, and the individual is responsible for the remaining 20%. However, if the individual has a secondary insurance plan, such as a Medigap plan, the secondary plan may cover some or all of the remaining 20%.
It is important for individuals to check with their healthcare provider and their insurance plan to determine the specific costs that they will be responsible for when it comes to catheter supplies.
Are There any Restrictions on How Often Medicare Will Cover Catheter Supplies?
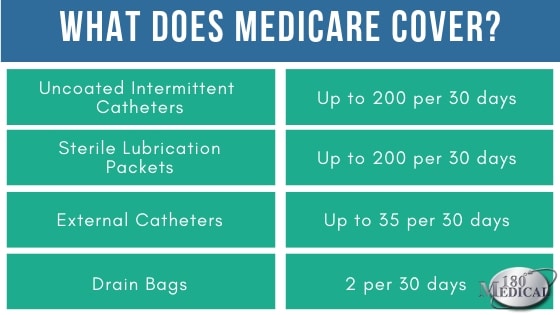
Medicare will cover catheter supplies as long as they are deemed medically necessary. However, there may be restrictions on how often Medicare will cover these supplies. For example, intermittent catheters may be covered up to 200 per month, while external catheters may be covered up to 35 per month.
It is important for individuals to talk to their healthcare provider to determine how often they will need catheter supplies, and to work with their supplier to ensure that they are receiving the appropriate amount of supplies each month.
Can I Purchase Catheter Supplies from any Supplier?
No, individuals must purchase catheter supplies from a supplier that is enrolled in Medicare and accepts Medicare assignment. This means that the supplier has agreed to accept the Medicare-approved amount as payment in full.
If an individual purchases catheter supplies from a supplier that is not enrolled in Medicare, they may be responsible for the full cost of the supplies. It is important to work with a supplier that is enrolled in Medicare to ensure that the individual is receiving the appropriate coverage and is not responsible for any unexpected costs.
In conclusion, Medicare does cover catheter supplies, but there are certain conditions that need to be met. Patients must have a medical need for the catheter, and it must be prescribed by a doctor. Additionally, the type of catheter and quantity needed must be deemed medically necessary.
It is important to note that while Medicare does cover catheter supplies, patients may still be responsible for certain out-of-pocket costs, such as deductibles and co-insurance. It is important for patients to understand their specific coverage and any potential costs before obtaining catheter supplies.
Overall, Medicare coverage for catheter supplies can provide much-needed relief for patients who require these essential medical devices. With the proper documentation and understanding of coverage, patients can access the supplies they need to manage their medical conditions and improve their quality of life.
Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior insurance, encompassing Medicare, Medigap, long-term care insurance, life insurance, and dental, vision, and hearing insurance. Vincent's unwavering passion for guiding seniors through the intricate insurance landscape and crafting customized solutions to address their individual needs has earned Over65InsuranceOptions an esteemed reputation as a dependable ally for seniors nationwide.
More Posts

