Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior...Read more
Introduction:
Rehabilitation is a crucial component of recovery for individuals struggling with addiction and other behavioral health disorders. However, the cost of rehab can be prohibitively expensive for many people. Medicare is a federal health insurance program that provides coverage for eligible individuals, but how long can a person stay in rehab on Medicare? In this article, we will explore the benefits of Medicare coverage for rehab and the duration of coverage that individuals can expect.
Paragraph 1:
Medicare is a valuable resource for individuals seeking treatment for addiction and other behavioral health disorders. Medicare Part A covers inpatient rehab services, including room and board, meals, and nursing care. However, the duration of coverage can vary depending on the individual’s needs and progress in treatment.
Paragraph 2:
In general, Medicare will cover up to 90 days of inpatient rehab per benefit period. If the individual requires additional treatment beyond this period, they may be eligible for up to 60 additional days of coverage, known as lifetime reserve days. It is important to note that not all rehab facilities accept Medicare, so it is essential to check with the facility before starting treatment.
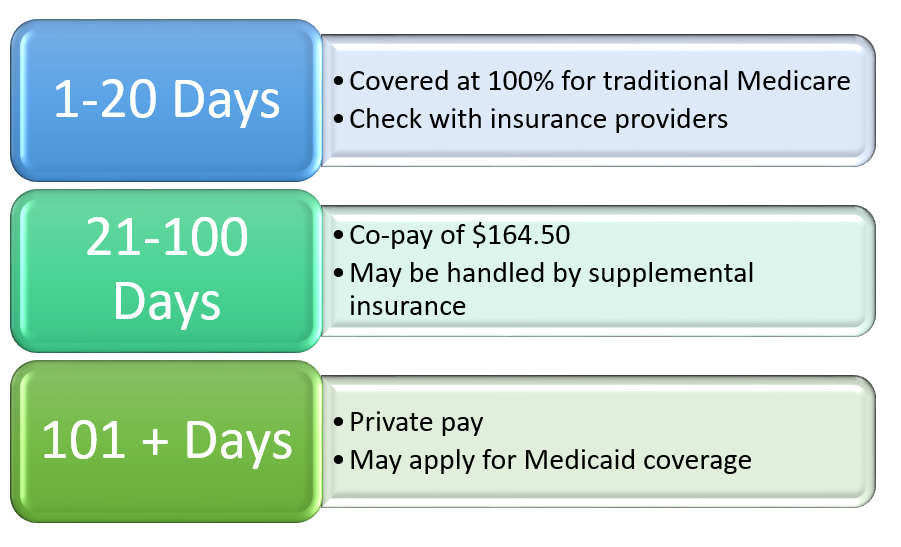
Medicare covers inpatient rehabilitation for up to 100 days per benefit period. However, to be eligible for coverage, the patient must have a qualifying hospital stay of at least three days and require skilled nursing or rehabilitation services. After the first 20 days, the patient may be responsible for a daily coinsurance payment.
How Long Can a Person Stay in Rehab on Medicare?
Rehabilitation programs can be incredibly helpful for individuals who are recovering from substance abuse, physical injuries, or other health-related issues. However, the cost of these programs can be a significant financial burden. For those who are eligible for Medicare, the question arises: how long can a person stay in rehab on Medicare? In this article, we will explore the answer to this question and provide additional information related to Medicare and rehabilitation programs.
Medicare Coverage for Rehabilitation Services
Medicare coverage for rehabilitation services varies depending on a person’s specific plan. However, in general, Medicare Part A covers inpatient rehabilitation services, including those related to substance abuse treatment or physical rehabilitation. Medicare Part B covers outpatient rehabilitation services, including physical therapy and speech therapy.
For inpatient rehabilitation services, Medicare Part A will cover up to 90 days in a psychiatric hospital during each benefit period. For substance abuse treatment, Medicare Part A will cover up to 190 days of inpatient care in a lifetime. However, these services must be deemed medically necessary by a healthcare provider.
For outpatient rehabilitation services, Medicare Part B will cover physical therapy, occupational therapy, and speech therapy. The amount of coverage will depend on the specific services received and the specific Medicare plan.
Medicare Advantage Plans and Rehabilitation Services
Medicare Advantage plans, also known as Medicare Part C, are offered by private insurance companies as an alternative to traditional Medicare. These plans may offer additional benefits, including coverage for rehabilitation services beyond what is covered by traditional Medicare.
For example, some Medicare Advantage plans may cover additional days of inpatient rehabilitation services beyond what is covered by traditional Medicare. Additionally, some plans may offer coverage for alternative therapies, such as acupuncture or chiropractic care, which may be helpful for individuals who are recovering from physical injuries.
Limitations of Medicare Coverage for Rehabilitation Services
While Medicare does provide coverage for rehabilitation services, there are some limitations to this coverage. For example, Medicare does not cover long-term care in a nursing home or assisted living facility. This means that individuals who require ongoing care may need to pay for these services out of pocket or seek alternative forms of coverage.
Additionally, the amount of coverage provided by Medicare may not be enough to cover the full cost of rehabilitation services. For example, Medicare may only cover a certain number of physical therapy sessions per year, which may not be enough for individuals who require ongoing care.
Benefits of Medicare Coverage for Rehabilitation Services
Despite the limitations of Medicare coverage for rehabilitation services, there are still many benefits to this coverage. For one, Medicare coverage can significantly reduce the cost of rehabilitation services for individuals who may not be able to afford these services otherwise. Additionally, Medicare coverage can provide access to high-quality rehabilitation programs that may not be available through other forms of insurance or out-of-pocket payment.
Alternatives to Medicare Coverage for Rehabilitation Services
For individuals who do not qualify for Medicare coverage or who require additional services beyond what is covered by Medicare, there are alternative forms of coverage available. For example, some private insurance plans may provide coverage for rehabilitation services, including those related to substance abuse treatment or physical rehabilitation.
Additionally, some state-run programs and nonprofit organizations may offer financial assistance for individuals who require rehabilitation services but cannot afford them. These programs and organizations may provide free or reduced-cost services, as well as transportation and other support services.
Conclusion
In conclusion, Medicare coverage for rehabilitation services can provide significant benefits for individuals who are recovering from substance abuse, physical injuries, or other health-related issues. While there are limitations to this coverage, including the length of coverage and the amount of coverage provided, Medicare can significantly reduce the cost of rehabilitation services for eligible individuals. For those who do not qualify for Medicare coverage, there are alternative forms of coverage available, including private insurance plans and state-run programs.
Frequently Asked Questions
Rehabilitation programs can help individuals overcome addiction and regain control of their lives. However, many people may be concerned about the cost and duration of rehab. If you have Medicare, you may be wondering about your coverage and how long you can stay in rehab. Here are some frequently asked questions about rehab and Medicare.
How long can a person stay in rehab on Medicare?
The length of time that a person can stay in rehab on Medicare can vary depending on the individual’s needs and the type of rehab program they are participating in. Medicare coverage for rehab typically includes up to 90 days of inpatient treatment. If necessary, Medicare may also cover an additional 60 days of inpatient treatment with a copayment. If you need additional treatment, you may be able to receive outpatient therapy or other services.
It is important to note that your doctor and the rehab center will determine the appropriate length of treatment based on your individual needs and progress. If you feel that you need more time in rehab, you should discuss this with your healthcare provider to see if additional coverage is available.
What types of rehab programs are covered by Medicare?
Medicare covers a variety of rehab programs, including inpatient and outpatient services. Inpatient rehab programs typically provide 24-hour care and support in a hospital or residential setting. Outpatient rehab programs allow individuals to receive treatment while living at home and may include individual or group therapy, medication management, or other services.
Medicare also covers specialized rehab programs for specific conditions, such as drug or alcohol addiction, mental health disorders, or physical rehabilitation. Your healthcare provider can help you determine which type of rehab program is best suited for your needs.
What is the cost of rehab on Medicare?
The cost of rehab on Medicare can vary depending on the type of program and the length of treatment. For inpatient rehab, Medicare typically covers all of the costs for the first 60 days and requires a copayment for days 61-90. For outpatient rehab, Medicare typically covers 80% of the cost, and you may be responsible for the remaining 20%.
It is important to note that some rehab centers may charge additional fees or have different cost structures. You should check with your healthcare provider and the rehab center to understand the full cost of treatment.
Before beginning rehab on Medicare, you may need to obtain prior authorization from Medicare. Your healthcare provider will need to provide documentation of your medical condition and the necessity of rehab treatment. If you do not obtain prior authorization, you may be responsible for the full cost of treatment.
It is important to work closely with your healthcare provider and Medicare to ensure that you have the necessary authorization and coverage for your rehab treatment.
Can I choose my own rehab center with Medicare?
Yes, you can choose your own rehab center with Medicare. However, it is important to choose a rehab center that is Medicare-certified to ensure that your treatment is covered by Medicare. You should also check with the rehab center to ensure that they accept Medicare and understand the costs and coverage of your treatment.
Your healthcare provider can provide you with a list of Medicare-certified rehab centers in your area and help you choose the best center for your needs.
In conclusion, the length of time a person can stay in rehab on Medicare varies based on their individual needs and progress in treatment. While Medicare provides coverage for up to 90 days of inpatient rehab care, individuals may be able to stay longer if they meet certain criteria. However, it is important to note that the goal of rehab is not just to stay as long as possible, but rather to make progress towards recovery and develop the skills necessary for long-term sobriety. Therefore, it is crucial for individuals and their healthcare providers to work together to create a personalized treatment plan that meets their specific needs and goals.
Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior insurance, encompassing Medicare, Medigap, long-term care insurance, life insurance, and dental, vision, and hearing insurance. Vincent's unwavering passion for guiding seniors through the intricate insurance landscape and crafting customized solutions to address their individual needs has earned Over65InsuranceOptions an esteemed reputation as a dependable ally for seniors nationwide.
More Posts

