Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior...Read more
As we age, healthcare becomes a crucial aspect of our lives. Medicare, a federal health insurance program, provides coverage to millions of Americans over the age of 65. However, not everyone is eligible for Medicare, and income plays a significant role in determining eligibility.
Many people wonder what the maximum income is to qualify for Medicare. The answer is not straightforward, as income limits vary depending on several factors, such as age, disability status, and marital status. In this article, we will explore the income limits for Medicare eligibility and provide insight into how to determine if you qualify.
What is the Maximum Income to Qualify for Medicare?
Medicare is a federal health insurance program that provides coverage for people who are 65 and older, as well as those with certain disabilities. It’s important to understand the rules and requirements for Medicare, including the maximum income to qualify. Here’s what you need to know.
1. Medicare Eligibility Based on Income
Medicare eligibility is based on age and disability, but it’s also based on income. If you’re 65 or older and have worked for at least 10 years, you’ll generally qualify for Medicare. However, if you have a high income, you may be subject to higher premiums.
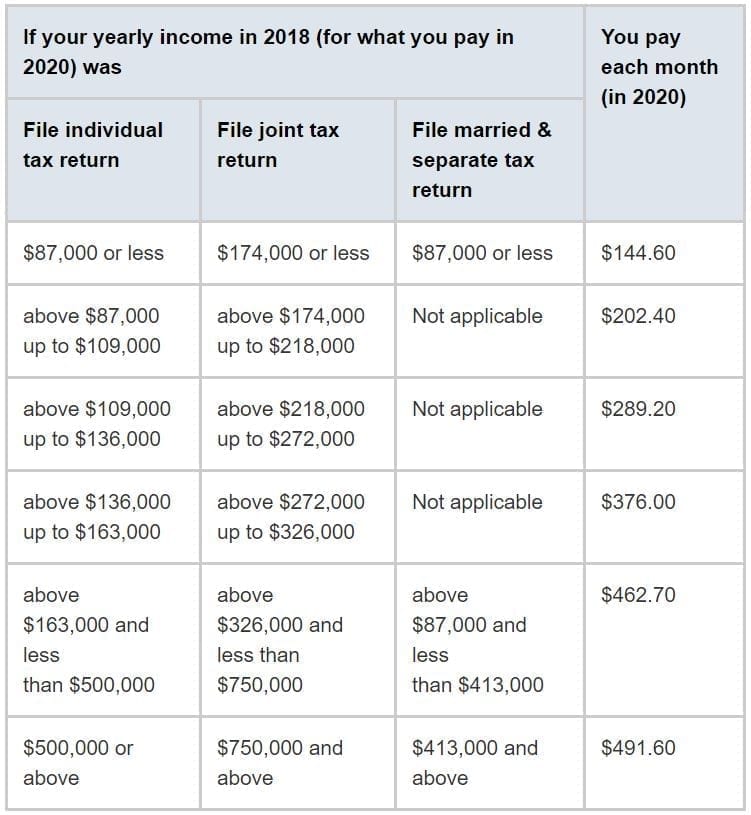
In general, individuals with a modified adjusted gross income (MAGI) of more than $88,000 and married couples filing jointly with a MAGI of more than $176,000 will pay higher premiums. These higher premiums are known as income-related monthly adjustment amounts (IRMAA).
2. Medicare Advantage and Supplemental Plans
If you’re worried about your income affecting your Medicare costs, you may want to consider Medicare Advantage or supplemental plans. Medicare Advantage plans are offered by private insurance companies and provide an alternative to traditional Medicare coverage. These plans often have lower out-of-pocket costs and may include additional benefits, such as vision or dental coverage.
Medicare supplemental plans, also known as Medigap policies, can help cover the cost of out-of-pocket expenses associated with traditional Medicare coverage. These policies are also offered by private insurance companies and can help you pay for deductibles, copayments, and coinsurance.
3. Benefits of Medicare
The benefits of Medicare are numerous. Medicare Part A covers hospital stays, skilled nursing care, and hospice care. Medicare Part B covers doctor visits, outpatient services, and preventive care. Medicare Part D provides coverage for prescription drugs.
In addition, Medicare Advantage plans and supplemental plans can provide additional benefits, such as dental, vision, and hearing coverage. These benefits can help you manage your healthcare costs and maintain your overall health and well-being.
4. Medicare vs. Medicaid
It’s important to understand the difference between Medicare and Medicaid. Medicare is a federal health insurance program that provides coverage for people who are 65 and older, as well as those with certain disabilities. Medicaid, on the other hand, is a joint federal-state program that provides coverage for low-income individuals and families.
If you’re eligible for both Medicare and Medicaid, you may be able to receive additional benefits, such as reduced premiums and lower out-of-pocket costs. It’s important to understand the rules and requirements for both programs to ensure that you’re getting the coverage you need.
5. How to Apply for Medicare
To apply for Medicare, you’ll need to fill out an application with the Social Security Administration. You can apply online, over the phone, or in person at your local Social Security office. It’s important to apply for Medicare during your initial enrollment period, which begins three months before your 65th birthday and ends three months after.
If you miss your initial enrollment period, you may be subject to a penalty. It’s important to understand the rules and requirements for Medicare enrollment to avoid any potential penalties or delays in coverage.
6. Medicare Enrollment Periods
In addition to your initial enrollment period, there are other enrollment periods for Medicare. The annual enrollment period runs from October 15 to December 7 each year and allows you to make changes to your Medicare coverage.
There’s also a special enrollment period for individuals who have lost their employer-sponsored health insurance. This enrollment period lasts for eight months after the loss of coverage and allows you to enroll in Medicare without penalty.
7. Medicare Open Enrollment
Medicare open enrollment is the time period when you can make changes to your Medicare coverage. This period runs from October 15 to December 7 each year. During this time, you can switch from traditional Medicare to Medicare Advantage, switch from one Medicare Advantage plan to another, or enroll in a Medicare prescription drug plan.
It’s important to review your Medicare coverage each year during open enrollment to ensure that you’re getting the coverage you need at a price you can afford.
8. Medicare Cost-Sharing
Medicare cost-sharing refers to the out-of-pocket expenses you’ll incur when receiving medical care. These expenses include deductibles, copayments, and coinsurance. Medicare supplemental plans can help cover these costs, but they can also be expensive.
It’s important to understand the cost-sharing requirements for Medicare and how they can affect your overall healthcare costs. Medicare Advantage plans may have lower cost-sharing requirements, but they may also have limits on which doctors and hospitals you can use.
9. Medicare and Pre-Existing Conditions
Medicare is required to cover pre-existing conditions, with a few exceptions. This means that even if you have a pre-existing condition, you’ll still be able to get coverage under Medicare.
It’s important to understand the rules and requirements for pre-existing conditions under Medicare to ensure that you’re getting the coverage you need. If you have a pre-existing condition, you may want to consider Medicare supplemental plans or Medicare Advantage plans to help cover the cost of your medical care.
10. Medicare and Long-Term Care
Medicare does not provide coverage for long-term care, such as nursing home care or assisted living facilities. If you need long-term care, you’ll need to pay for it out of pocket or through long-term care insurance.
It’s important to plan for long-term care expenses as you age, as these expenses can be quite high. Medicare supplemental plans and Medicare Advantage plans may provide some coverage for long-term care, but it’s important to understand the limitations of this coverage.
In conclusion, understanding the maximum income to qualify for Medicare is an important part of planning for your healthcare costs in retirement. By understanding the rules and requirements for Medicare, you can ensure that you’re getting the coverage you need at a price you can afford.
Contents
Frequently Asked Questions
1. What is the maximum income to qualify for Medicare?
To qualify for Medicare, there is no maximum income limit. Eligibility for Medicare is primarily based on age and disability status. Individuals who are 65 years or older and have paid into Medicare through payroll taxes for at least 10 years are generally eligible for Medicare Part A, which covers hospitalization. Medicare Part B, which covers doctor visits and other outpatient services, is also available to those who are eligible for Part A and pay a monthly premium.
Yes, there are income limits for Medicare Part B premiums. The amount you pay for Part B depends on your income level. The standard monthly premium for 2021 is $148.50, but individuals with higher incomes may pay more. The income brackets for 2021 range from $88,000 to $500,000 or more for individuals, and $176,000 to $750,000 or more for married couples filing jointly.
Income for Medicare premium purposes is determined by your modified adjusted gross income (MAGI). MAGI is calculated by taking your adjusted gross income (AGI) and adding back certain deductions, such as tax-exempt interest. Your MAGI is then used to determine which income bracket you fall into for Medicare premium purposes.
4. What happens if my income changes during the year?
If your income changes during the year and you are paying a higher premium than you should be based on your new income level, you can request an adjustment. This is known as a Medicare Income-Related Monthly Adjustment Amount (IRMAA) Reconsideration. You will need to provide documentation of your new income level to the Social Security Administration, which administers Medicare.
5. Are there any programs to help low-income individuals with Medicare costs?
Yes, there are several programs available to help low-income individuals with Medicare costs. The most well-known program is the Medicare Savings Program (MSP), which helps pay for Medicare premiums and, in some cases, Medicare deductibles and co-payments. There is also the Extra Help program, which helps pay for prescription drug costs under Medicare Part D. Both programs have income and asset limits, and eligibility varies by state.
In conclusion, the maximum income to qualify for Medicare depends on several factors, including age, disability status, and income level. For those who are 65 or older and have worked for at least 10 years, there is no income limit to qualify for Medicare Part A, which covers hospital stays and some post-hospital care.
However, for Medicare Part B, which covers doctor visits and other outpatient services, there is an income-based premium. The income threshold for this premium varies depending on the individual’s tax filing status and income level.
Additionally, those with disabilities and certain medical conditions may also qualify for Medicare, regardless of their income level. It’s important to review your eligibility requirements and speak with a qualified healthcare professional to determine your specific Medicare coverage options.
Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior insurance, encompassing Medicare, Medigap, long-term care insurance, life insurance, and dental, vision, and hearing insurance. Vincent's unwavering passion for guiding seniors through the intricate insurance landscape and crafting customized solutions to address their individual needs has earned Over65InsuranceOptions an esteemed reputation as a dependable ally for seniors nationwide.
More Posts

