Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior...Read more
Medicare is a federally funded healthcare program that provides health insurance coverage to individuals aged 65 or older, younger people with disabilities, and people with end-stage renal disease. One of the benefits of Medicare is its coverage for rehabilitation services, but how long will Medicare pay for rehab?
That’s a question that many people ask, and the answer can be complicated. In this article, we will explore the different types of rehabilitation services covered by Medicare, how long Medicare will pay for these services, and what factors can affect your coverage.
Medicare will pay for up to 100 days of rehabilitation services in a skilled nursing facility per benefit period. However, to qualify for Medicare coverage, patients must have been hospitalized for at least three days and require skilled nursing care or therapy services. After the first 20 days, a daily coinsurance fee may be required.
How Many Days Will Medicare Pay for Rehab?
If you or a loved one needs rehabilitation services, you may be wondering how long Medicare will cover the costs. Medicare is a federal health insurance program that provides coverage for people who are 65 or older, younger people with disabilities, and people with end-stage renal disease. Medicare covers a wide range of services, including rehabilitation services. However, the number of days that Medicare will pay for rehab can vary depending on several factors.
1. Inpatient Rehabilitation
Inpatient rehabilitation is a type of rehab service that requires you to stay in a hospital or a specialized rehabilitation facility. Medicare Part A covers inpatient rehabilitation services, including room and board, meals, nursing care, and therapy services. Medicare will cover up to 100 days of inpatient rehabilitation per benefit period. However, not all patients will qualify for the full 100 days of coverage.
To qualify for inpatient rehabilitation, you must have a qualifying hospital stay of at least three days, and your doctor must certify that you need inpatient rehabilitation. Your doctor must also develop a plan of care for your rehabilitation, and you must participate in and make progress towards your rehabilitation goals.
2. Outpatient Rehabilitation
Outpatient rehabilitation is a type of rehab service that does not require you to stay in a hospital or a specialized rehabilitation facility. Instead, you can receive therapy services on an outpatient basis, either at a hospital, a rehabilitation agency, or a private practice. Medicare Part B covers outpatient rehabilitation services, including physical therapy, occupational therapy, and speech therapy.
Medicare will pay for outpatient rehabilitation services as long as they are medically necessary and provided by a qualified healthcare provider. There is no limit to the number of outpatient rehabilitation services that Medicare will cover, but you may have to pay a copayment or coinsurance for each service.
3. Skilled Nursing Facility Rehabilitation
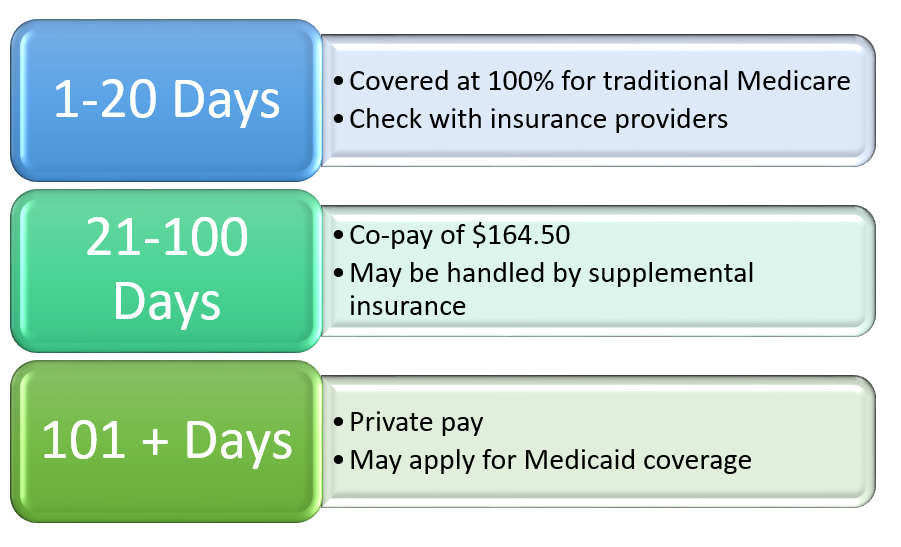
Skilled nursing facility (SNF) rehabilitation is a type of rehab service that is provided in a nursing home or a skilled nursing facility. Medicare Part A covers SNF rehabilitation services, including room and board, nursing care, and therapy services. Medicare will cover up to 100 days of SNF rehabilitation per benefit period.
To qualify for SNF rehabilitation, you must have a qualifying hospital stay of at least three days, and your doctor must certify that you need SNF rehabilitation. Your doctor must also develop a plan of care for your rehabilitation, and you must participate in and make progress towards your rehabilitation goals. However, not all patients will qualify for the full 100 days of coverage.
4. Home Health Rehabilitation
Home health rehabilitation is a type of rehab service that is provided in your home by a qualified healthcare provider. Medicare Part A and Part B cover home health rehabilitation services, including physical therapy, occupational therapy, and speech therapy.
Medicare will pay for home health rehabilitation services as long as they are medically necessary and provided by a qualified healthcare provider. There is no limit to the number of home health rehabilitation services that Medicare will cover, but you may have to pay a copayment or coinsurance for each service.
5. Rehabilitation Benefits
Rehabilitation benefits under Medicare can help you recover from an injury or illness and improve your quality of life. Rehabilitation services can help you regain your strength, mobility, and independence, and reduce your risk of future complications. Rehabilitation services can also help you manage chronic conditions and prevent further decline.
If you need rehabilitation services, it is important to understand your benefits under Medicare and work with your healthcare providers to develop a plan of care that meets your needs. You may also want to consider supplemental insurance or other options to help cover the costs of your care.
6. Rehabilitation Vs. Long-Term Care
Rehabilitation services are different from long-term care services, which are designed to help people with chronic conditions or disabilities who need ongoing assistance with daily activities. Long-term care services can include nursing home care, assisted living, and home health aide services.
Medicare does not cover long-term care services, except in limited circumstances. If you need long-term care services, you may need to rely on other sources of funding, such as Medicaid, private insurance, or out-of-pocket payments.
7. Rehabilitation Vs. Hospice Care
Rehabilitation services are also different from hospice care, which is designed to provide comfort and support to people who are terminally ill or have a life-limiting illness. Hospice care focuses on relieving pain and symptoms and improving the quality of life for patients and their families.
Medicare covers hospice care under Part A, but only if your doctor certifies that you have a life expectancy of six months or less. Hospice care can include a range of services, such as nursing care, medical equipment, and counseling services.
8. Choosing a Rehabilitation Provider
If you need rehabilitation services, it is important to choose a qualified provider who can meet your needs and provide high-quality care. You may want to ask your doctor for recommendations, or research providers in your area online.
When choosing a rehabilitation provider, consider factors such as their experience, qualifications, and reputation. You may also want to ask about their approach to care, their availability, and their fees and payment options.
9. Paying for Rehabilitation Services
Medicare will cover a portion of the costs of your rehabilitation services, but you may still be responsible for some out-of-pocket expenses, such as copayments or coinsurance. If you have supplemental insurance, such as a Medigap policy, it may help cover some of these costs.
If you do not have supplemental insurance, you may need to pay for some of your rehabilitation costs out of pocket. You may also be able to negotiate a payment plan with your provider, or seek financial assistance from other sources, such as charitable organizations or state programs.
10. Conclusion
Rehabilitation services can be an important part of your recovery from an injury or illness. Medicare provides coverage for a range of rehabilitation services, including inpatient rehabilitation, outpatient rehabilitation, skilled nursing facility rehabilitation, and home health rehabilitation. The number of days that Medicare will pay for rehab can vary depending on several factors, such as the type of service and your individual needs.
If you need rehabilitation services, it is important to work with your healthcare providers to develop a plan of care that meets your needs and fits within your Medicare coverage. You may also want to consider supplemental insurance or other options to help cover the costs of your care.
Contents
Frequently Asked Questions
Medicare provides coverage for rehabilitation services to individuals who are eligible for the benefits. However, many people are unsure about how long Medicare will pay for rehab. Here are some common questions and answers regarding Medicare coverage for rehab:
How long will Medicare pay for inpatient rehab?
Medicare will pay for inpatient rehabilitation for up to 100 days per benefit period. However, not all patients will qualify for the full 100 days of coverage. The patient must have a qualifying hospital stay of at least three days and require skilled nursing care or other rehabilitative services that can only be provided in a skilled nursing facility or rehab hospital.
After the first 20 days, there may be a daily copayment required. If the patient exhausts their 100 days of coverage, they will be responsible for all costs associated with their care.
How long will Medicare pay for outpatient rehab?
Medicare will pay for outpatient rehabilitation services as long as the services are medically necessary and deemed reasonable and necessary by the patient’s healthcare provider. There is no set limit on the number of days or visits that Medicare will cover for outpatient rehab services.
However, there may be limits on the amount of therapy services that are covered each year. Patients should check with their healthcare provider or Medicare to determine their coverage limits.
What types of rehab services are covered by Medicare?
Medicare will cover a wide range of rehab services, including physical therapy, occupational therapy, and speech therapy. Medicare will also cover skilled nursing care and other rehabilitative services that are deemed medically necessary by the patient’s healthcare provider.
It is important to note that Medicare will only cover services that are considered reasonable and necessary for the treatment of the patient’s condition. Patients should work closely with their healthcare provider to determine which services are covered under their Medicare plan.
Does Medicare cover the cost of home health rehabilitation services?
Yes, Medicare will cover the cost of home health rehabilitation services as long as the services are deemed medically necessary and reasonable by the patient’s healthcare provider. Home health rehab services may include physical therapy, occupational therapy, and speech therapy.
Patients must meet certain eligibility criteria to qualify for home health services, including being homebound and requiring skilled nursing care or rehabilitative services that can only be provided in a home setting.
Can patients receive rehab services from non-Medicare providers?
Yes, patients can receive rehab services from non-Medicare providers. However, Medicare will only cover services that are deemed medically necessary and reasonable by the patient’s healthcare provider. Patients should work closely with their healthcare provider and non-Medicare providers to ensure that the services they receive are covered under their Medicare plan.
Patient may be responsible for paying any costs associated with non-Medicare providers that are not covered under their Medicare plan.
In conclusion, Medicare coverage for rehabilitation services is based on a variety of factors, including the type of care needed, the individual’s health condition, and the length of time required to achieve maximum health benefits. While Medicare may cover up to 100 days of rehabilitation services, it is important to understand that this coverage is not automatic and may require additional documentation and approvals.
It is important to work closely with healthcare providers and caregivers to ensure that all necessary steps are taken to maximize Medicare coverage for rehabilitation services. This may include obtaining referrals, completing assessments, and providing documentation to demonstrate the medical necessity of rehabilitation services.
Ultimately, the goal of Medicare coverage for rehabilitation services is to help individuals achieve the best possible health outcomes and improve their quality of life. By working closely with healthcare providers and taking advantage of available resources, individuals can maximize their Medicare coverage and receive the care they need to achieve their health goals.
Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior insurance, encompassing Medicare, Medigap, long-term care insurance, life insurance, and dental, vision, and hearing insurance. Vincent's unwavering passion for guiding seniors through the intricate insurance landscape and crafting customized solutions to address their individual needs has earned Over65InsuranceOptions an esteemed reputation as a dependable ally for seniors nationwide.
More Posts

