Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior...Read more
As we grow older, it’s important to consider our healthcare options to ensure we receive the best care possible. One option available for seniors is Medicare, which can provide coverage for a variety of medical services, including nursing home care. However, it’s important to understand the limitations and duration of Medicare coverage for nursing home care.
So, how many days does Medicare pay for nursing home care? This is a common question among seniors and their families. In this article, we’ll explore the details of Medicare coverage for nursing home care and provide helpful information to help you make informed decisions about your healthcare options.
How Many Days Does Medicare Pay for Nursing Home?
If you or a loved one needs to stay in a nursing home, it’s important to understand how Medicare will cover the costs. Medicare is a federal health insurance program that primarily covers people over the age of 65, as well as those with certain disabilities. While Medicare does cover some costs associated with nursing home care, it’s important to note that it doesn’t cover everything. Here’s what you need to know about how many days Medicare will pay for nursing home care.
Medicare Coverage for Nursing Home Care
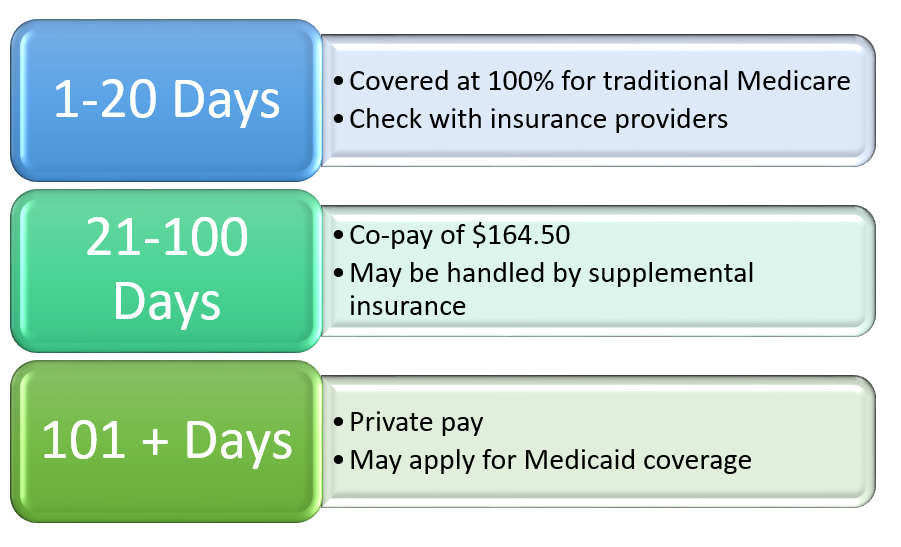
Medicare Part A covers some of the costs associated with nursing home care, but only for a limited time. If you meet certain criteria, Medicare will cover up to 100 days of skilled nursing facility (SNF) care per benefit period. To be eligible for this coverage, you must have spent at least three consecutive days in the hospital and require skilled care that can only be provided in a nursing home.
During the first 20 days of your stay, Medicare will cover the full cost of your care. For days 21 through 100, there is a daily coinsurance amount that you will be responsible for paying. In 2021, the daily coinsurance amount is $185.50. After 100 days, Medicare will no longer cover your nursing home care.
What is Skilled Nursing Facility (SNF) Care?
Skilled nursing facility (SNF) care is a type of nursing home care that is provided by skilled nursing staff, such as registered nurses (RNs) and licensed practical nurses (LPNs). This type of care is typically required for patients who have complex medical needs or who require a high level of care.
To qualify for SNF care under Medicare, you must require daily skilled care that can only be provided by or under the supervision of professional medical personnel. Examples of skilled care include wound care, physical therapy, and intravenous injections.
Are There Any Exceptions to the 100-Day Limit?
There are some exceptions to the 100-day limit on Medicare coverage for nursing home care. If you leave the nursing home for at least 60 consecutive days, your benefit period will reset. This means that if you need to return to the nursing home after that time, you will be eligible for another 100 days of coverage.
Additionally, if your doctor certifies that you require continued skilled care after the 100-day limit has been reached, you may be eligible for an extension of coverage. However, these extensions are typically only granted in exceptional circumstances.
What Are the Other Costs of Nursing Home Care?
While Medicare covers some of the costs associated with nursing home care, it doesn’t cover everything. There may be other costs that you will need to pay for out of pocket or through other insurance programs. Some of the costs that you may be responsible for include:
- Room and board
- Personal care items, such as toiletries and clothing
- Medical supplies and equipment
- Prescription medications
What Are the Alternatives to Nursing Home Care?
If you or a loved one require care but don’t want to stay in a nursing home, there are other options available. Some of these alternatives include:
- Home health care
- Hospice care
- Assisted living facilities
- Adult day care
Each of these options has its own benefits and drawbacks, so it’s important to do your research before making a decision.
Conclusion
Medicare does provide coverage for some of the costs associated with nursing home care, but only for a limited time. Understanding how long Medicare will pay for nursing home care can help you plan for the future and ensure that you or your loved one receives the care they need. If you have any questions about Medicare coverage for nursing home care, be sure to talk to your healthcare provider or a Medicare representative.
Frequently Asked Questions
How Many Days Does Medicare Pay for Nursing Home?
Medicare will pay for up to 100 days of skilled nursing care in a nursing home facility. However, there are some limitations and restrictions to this coverage. To be eligible for this coverage, the patient must have been admitted to the hospital for at least three days, and then transferred to a Medicare-certified skilled nursing facility within 30 days of their hospitalization. Additionally, the patient must require skilled nursing care, such as physical therapy, speech therapy, or occupational therapy, on a daily basis.
It’s important to note that Medicare will cover the full cost of care for the first 20 days in a skilled nursing facility. After the first 20 days, there may be a daily copayment required, which the patient or their insurance would be responsible for. If the patient requires care beyond the 100-day limit, they would need to pay out of pocket or rely on other insurance policies, such as long-term care insurance.
What Happens After Medicare Coverage Ends?
After Medicare coverage ends, the patient or their family would need to consider other options for long-term care. This may include paying out of pocket for care, relying on long-term care insurance, or qualifying for Medicaid. Medicaid is a government-funded program that provides assistance for individuals who have low income and limited resources. To be eligible for Medicaid, the patient would need to meet certain income and asset requirements, which vary by state.
It’s important to begin planning for long-term care well before the Medicare coverage ends. This may include researching different long-term care options, such as assisted living facilities or in-home care, and determining the costs associated with each option. Additionally, it may be beneficial to speak with a financial planner or elder law attorney to discuss financial planning strategies and legal options for long-term care.
Does Medicare Cover Assisted Living Facilities?
Medicare does not typically cover the cost of assisted living facilities. Assisted living facilities provide a lower level of care than skilled nursing facilities, and are designed for individuals who need assistance with daily activities, such as dressing, bathing, and medication management. Medicare may cover some medical services that are provided within an assisted living facility, such as physical therapy or occupational therapy, but it does not cover the cost of room and board or other non-medical services.
There are other insurance options that may provide coverage for assisted living facilities, such as long-term care insurance or Medicaid. Additionally, some states offer Medicaid waiver programs that provide assistance for individuals who would otherwise require skilled nursing care in a nursing home, but are able to receive care in an assisted living facility.
What Is the Difference Between Skilled Nursing Care and Custodial Care?
Skilled nursing care refers to medical care that is provided by licensed medical professionals, such as registered nurses or physical therapists. This type of care is typically required for individuals who have a medical condition or injury that requires ongoing medical attention, such as wound care or rehabilitation services. Skilled nursing care is covered by Medicare for up to 100 days, as long as the patient meets certain requirements.
Custodial care, on the other hand, refers to non-medical care that is provided by caregivers or aides, such as assistance with daily activities like bathing, dressing, and eating. Custodial care is not covered by Medicare, and is typically paid for out of pocket or through long-term care insurance. It’s important to note that some individuals may require both skilled nursing care and custodial care, depending on their medical condition and level of independence.
How Can I Find a Medicare-Certified Nursing Home?
To find a Medicare-certified nursing home in your area, you can use the Medicare Nursing Home Compare tool on the Medicare website. This tool allows you to search for nursing homes by location, and provides information on the quality of care, staffing levels, and other important factors. Additionally, you can speak with your healthcare provider or social worker for recommendations on nursing homes in your area. It’s important to visit the nursing homes in person and ask questions about their services and policies before making a decision.
In conclusion, the number of days that Medicare pays for nursing home care varies depending on certain factors. It is essential to understand that Medicare only covers skilled nursing care and not long-term care.
On average, Medicare covers up to 100 days of skilled nursing care per benefit period. However, this coverage is subject to certain conditions, such as hospitalization for at least three days and a doctor’s order for skilled nursing care.
It is also important to note that Medicare coverage for nursing home care is limited, and patients may have to pay out-of-pocket for some services. Therefore, it is advisable to consult with a healthcare professional or a Medicare specialist to determine the best course of action for your specific situation.
Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior insurance, encompassing Medicare, Medigap, long-term care insurance, life insurance, and dental, vision, and hearing insurance. Vincent's unwavering passion for guiding seniors through the intricate insurance landscape and crafting customized solutions to address their individual needs has earned Over65InsuranceOptions an esteemed reputation as a dependable ally for seniors nationwide.
More Posts

