Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior...Read more
Medicare Secondary Payer is a term that is often heard in the world of healthcare. It refers to a set of rules that determine whether Medicare or another insurer is responsible for paying for medical treatment. This can be a confusing topic, but understanding it is essential for anyone who is eligible for Medicare or who provides healthcare services to Medicare beneficiaries.
In this article, we will explore what Medicare Secondary Payer is, when it applies, and what it means for patients and healthcare providers. Whether you are a Medicare beneficiary, a healthcare provider, or just someone interested in healthcare policy, this article will provide you with a clear understanding of this important topic. So, let’s dive in!
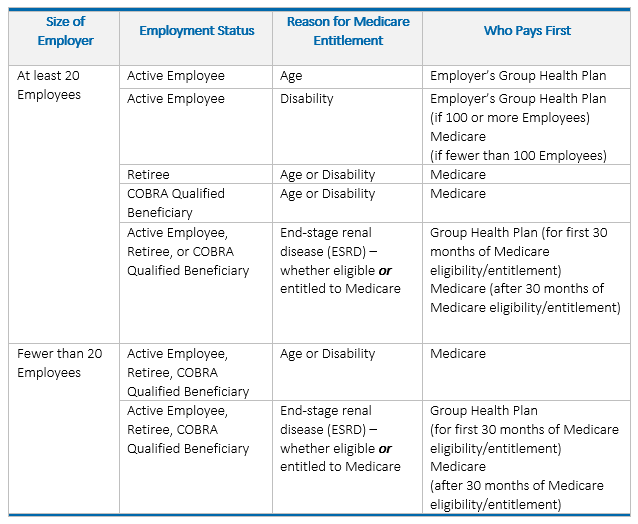
Medicare Secondary Payer (MSP) is a federal law that requires certain group health plans to pay secondary to Medicare. The law applies to group health plans of employers with 20 or more employees, and to employee health plans of employers with fewer than 20 employees if the employee is also covered by Medicare due to age or disability. The purpose of MSP is to ensure that Medicare does not pay for healthcare services that should be covered by other insurance plans.
When is Medicare Secondary Payer?
Medicare Secondary Payer (MSP) refers to the situations in which Medicare is not the primary payer of healthcare costs. Instead, another entity, such as an employer group health plan or a workers’ compensation plan, is responsible for paying for healthcare services first. In these cases, Medicare serves as the secondary payer.
What is Medicare Secondary Payer?
Medicare is a federal healthcare program that provides coverage for individuals who are 65 or older, as well as for younger individuals with certain disabilities or medical conditions. However, in certain situations, Medicare is not the primary payer of healthcare costs. In these cases, another entity is responsible for paying first. This entity is referred to as the primary payer.
There are several situations in which Medicare may be the secondary payer. For example, if an individual is covered by an employer group health plan, the health plan would be the primary payer for any healthcare services received. Medicare would then serve as the secondary payer, covering any costs that the health plan does not cover.
Another situation in which Medicare may be the secondary payer is if an individual is injured on the job and receives workers’ compensation benefits. In this case, the workers’ compensation plan would be the primary payer for any healthcare services related to the injury. Medicare would then serve as the secondary payer, covering any costs that the workers’ compensation plan does not cover.
Benefits of Medicare Secondary Payer
There are several benefits to the Medicare Secondary Payer program. For one, it helps ensure that healthcare costs are paid appropriately. If Medicare were always the primary payer, it could result in overpayments and unnecessary costs. By allowing other entities to serve as the primary payer in certain situations, the program helps ensure that Medicare is only paying for healthcare costs that it is responsible for.
Additionally, the program helps protect the Medicare Trust Fund. By having other entities serve as the primary payer in certain situations, Medicare is able to conserve its resources and ensure that they are being used appropriately.
Medicare Secondary Payer vs. Other Payer Programs
The Medicare Secondary Payer program is not the only program of its kind. There are other payer programs, such as the Coordination of Benefits (COB) program, that operate similarly. However, there are some key differences between these programs.
The COB program applies when an individual has more than one insurance plan that covers the same healthcare services. In these cases, the plans coordinate to determine which plan is responsible for paying first and which plan is responsible for paying second. Medicare may be involved in the COB program if an individual has both Medicare and another insurance plan.
How Medicare Secondary Payer Works
When Medicare is the secondary payer, it typically pays for healthcare costs that the primary payer does not cover. For example, if an individual has a health plan that covers 80% of healthcare costs and Medicare is the secondary payer, Medicare would cover the remaining 20% of costs.
In order for Medicare to serve as the secondary payer, the primary payer must be notified of the individual’s Medicare coverage. This is typically done by the healthcare provider. Once the primary payer has been notified, they will process the claim and pay for healthcare costs as appropriate. Medicare will then be billed for any costs that the primary payer did not cover.
When Medicare is Not the Secondary Payer
There are some situations in which Medicare is not the secondary payer. For example, if an individual is covered by Medicaid, Medicaid is the primary payer for any healthcare services received. Medicare would not be involved in this situation.
Additionally, if an individual has coverage through the Veterans Health Administration (VA), the VA is responsible for paying for any healthcare services received. Medicare would not be involved in this situation either.
Conclusion
The Medicare Secondary Payer program is an important part of the Medicare system. By allowing other entities to serve as the primary payer in certain situations, the program helps ensure that healthcare costs are paid appropriately and that the Medicare Trust Fund is protected. Understanding how the program works can help individuals make informed decisions about their healthcare coverage.
Contents
- Frequently Asked Questions
- What is Medicare Secondary Payer?
- When is Medicare Secondary Payer applicable?
- What are the penalties for non-compliance with Medicare Secondary Payer rules?
- How can healthcare providers and insurers ensure compliance with Medicare Secondary Payer rules?
- What are the benefits of complying with Medicare Secondary Payer rules?
Frequently Asked Questions
What is Medicare Secondary Payer?
Medicare Secondary Payer (MSP) is a term that refers to situations where Medicare is not the primary payer of healthcare expenses. In these cases, another entity, such as an employer group health plan or worker’s compensation plan, is responsible for paying the medical expenses first. Medicare is then responsible for paying any remaining costs.
The MSP rules are designed to ensure that Medicare does not pay for healthcare expenses that should be covered by another entity, protecting the Medicare trust fund from unnecessary spending.
When is Medicare Secondary Payer applicable?
Medicare Secondary Payer rules apply in situations where Medicare is not the primary payer of healthcare expenses. This can occur in several situations, including when an individual has group health insurance through their employer or when they receive worker’s compensation benefits.
Other situations where MSP rules may apply include when an individual is involved in a lawsuit or when they receive benefits from a no-fault insurance policy.
What are the penalties for non-compliance with Medicare Secondary Payer rules?
Non-compliance with MSP rules can result in serious penalties for healthcare providers, insurers, and other entities responsible for paying medical expenses. These penalties can include fines, legal action, and exclusion from participating in Medicare and other federal healthcare programs.
To avoid these penalties, it is important to understand and comply with MSP rules and regulations. Healthcare providers and insurers should ensure that they are properly identifying situations where MSP rules apply and taking appropriate action to comply with these rules.
How can healthcare providers and insurers ensure compliance with Medicare Secondary Payer rules?
To ensure compliance with MSP rules, healthcare providers and insurers should implement policies and procedures to identify situations where MSP rules apply and take appropriate action to comply with these rules.
This may include coordinating with other entities responsible for paying medical expenses, such as employer group health plans or worker’s compensation plans, to ensure that these entities are paying the appropriate share of healthcare costs before Medicare pays any remaining costs.
What are the benefits of complying with Medicare Secondary Payer rules?
Complying with MSP rules can help healthcare providers and insurers avoid serious penalties, such as fines and legal action, and maintain their eligibility to participate in Medicare and other federal healthcare programs.
In addition, complying with MSP rules can help protect the Medicare trust fund from unnecessary spending and ensure that individuals receive the appropriate level of healthcare coverage and benefits.
In conclusion, Medicare Secondary Payer (MSP) is a term used to describe the situation where Medicare is not the primary payer for a healthcare claim. Instead, another insurance provider or entity is responsible for paying for the medical expenses first. This can happen in various situations, such as when a person has group health insurance through their employer or when a personal injury claim is involved.
It is important to understand when MSP applies, as it can affect the amount of reimbursement a person receives for their healthcare expenses. Failing to comply with MSP requirements can also result in penalties and legal consequences.
Overall, navigating the world of healthcare and insurance can be complex, but understanding MSP and its implications is crucial for individuals and healthcare providers alike. By staying informed and following the necessary guidelines, we can ensure that healthcare expenses are appropriately covered and managed.
Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior insurance, encompassing Medicare, Medigap, long-term care insurance, life insurance, and dental, vision, and hearing insurance. Vincent's unwavering passion for guiding seniors through the intricate insurance landscape and crafting customized solutions to address their individual needs has earned Over65InsuranceOptions an esteemed reputation as a dependable ally for seniors nationwide.
More Posts

