Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior...Read more
Medicare is a government-funded healthcare program that provides coverage for millions of Americans. One of the benefits that Medicare offers is coverage for rehabilitation services. However, many people are left wondering how long Medicare will pay for rehab. This topic is important because it can impact the quality of care that individuals receive and their overall healthcare costs.
The answer to this question is not straightforward, as it depends on several factors, such as the type of rehab needed and the individual’s healthcare needs. In this article, we will explore the details of Medicare’s coverage for rehabilitation services and provide helpful information for those seeking rehab services.
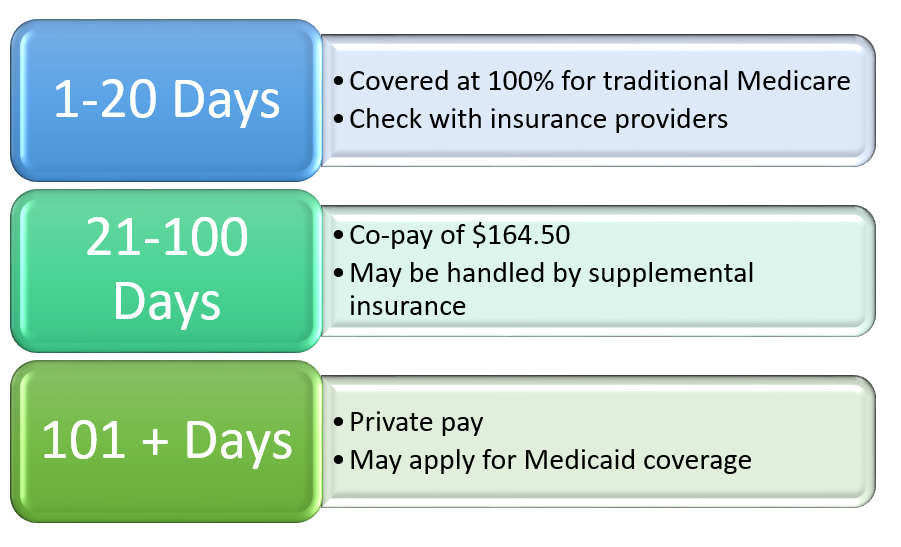
Medicare typically covers up to 100 days of inpatient rehabilitation care per benefit period. However, there are certain conditions that must be met in order to qualify for coverage beyond the initial 20 days. The patient must continue to show improvement and require skilled care, and they must have a three-day qualifying hospital stay prior to admission to the rehab facility. It’s important to note that Medicare may not cover the full cost of rehabilitation care, and patients may be responsible for co-payments or deductibles.
How Long Will Medicare Pay for Rehab?
Medicare is a federal program that provides health insurance for individuals aged 65 years and above, as well as those with certain disabilities. One of the benefits of Medicare is its coverage for rehabilitation services. However, many people wonder how long Medicare will pay for rehab. In this article, we will explore the different factors that influence the duration of Medicare coverage for rehab.
1. The Type of Rehab Services
The type of rehab services you require will determine how long Medicare will cover your rehab. There are different types of rehab services, including physical therapy, occupational therapy, and speech therapy. The duration of coverage for each type of rehab service may vary.
For physical therapy, Medicare will cover up to 100% of the cost for the first 20 days of rehab. From days 21 to 100, Medicare will cover 80% of the cost, and you will be responsible for the remaining 20%. If you require rehab beyond 100 days, Medicare will no longer cover the cost.
On the other hand, Medicare will cover occupational therapy and speech therapy to the same extent as physical therapy. However, there is no limit on the duration of coverage for these types of rehab services.
2. Your Medical Condition
Your medical condition is another factor that influences how long Medicare will pay for rehab. If you have a chronic condition that requires ongoing rehab, Medicare may cover the cost for an extended period. For example, if you have Parkinson’s disease and require physical therapy to manage your symptoms, Medicare may cover the cost for an indefinite period.
However, if your medical condition improves, and you no longer require rehab services, Medicare will no longer cover the cost. Medicare only covers rehab services that are deemed medically necessary.
3. Medicare Part A vs. Part B Coverage
Medicare Part A and Part B offer different coverage for rehab services. Part A covers inpatient rehab services, while Part B covers outpatient rehab services. The duration of coverage may vary depending on whether you are receiving inpatient or outpatient rehab services.
For inpatient rehab services, Medicare will cover up to 100% of the cost for the first 60 days. From days 61 to 90, you will be responsible for a daily coinsurance amount. From days 91 to 150, you will be responsible for a higher daily coinsurance amount. Beyond 150 days, Medicare will no longer cover the cost.
For outpatient rehab services, Medicare will cover up to 80% of the cost. You will be responsible for the remaining 20%. There is no limit on the duration of coverage for outpatient rehab services.
4. The Rehab Facility
The rehab facility you choose may also influence how long Medicare will pay for rehab. Medicare only covers rehab services provided by certified rehab facilities. If you choose a non-certified rehab facility, Medicare will not cover the cost.
Additionally, the type of rehab facility may also influence the duration of coverage. For example, if you require rehab services in a hospital setting, Medicare may cover the cost for an extended period. However, if you receive rehab services in a skilled nursing facility, the duration of coverage may be limited.
5. Your Medicare Coverage
Your Medicare coverage may also influence how long Medicare will pay for rehab. If you have a Medicare Advantage plan, your coverage for rehab services may differ from the coverage offered by Original Medicare. It’s essential to understand your Medicare coverage and the limitations associated with your plan.
In summary, the duration of Medicare coverage for rehab services may vary depending on several factors. These factors include the type of rehab services, your medical condition, Medicare Part A vs. Part B coverage, the rehab facility, and your Medicare coverage. It’s essential to consult with your healthcare provider and Medicare to understand the duration of coverage for your specific rehab needs.
Contents
- Frequently Asked Questions
- Q: How long will Medicare pay for rehab?
- Q: What happens if I don’t meet Medicare’s requirements for rehab coverage?
- Q: Can I switch from inpatient rehab to outpatient rehab if I’m not making progress?
- Q: What types of rehab services does Medicare cover?
- Q: How do I know if I’m eligible for Medicare rehab coverage?
Frequently Asked Questions
Q: How long will Medicare pay for rehab?
A: Medicare will pay for inpatient rehab for up to 100 days, but only if you meet certain requirements. First, you must have been hospitalized for at least three consecutive days. Second, your doctor must certify that you need daily skilled care, such as physical therapy or speech therapy. Finally, you must be making progress towards your goals.
However, it’s important to note that Medicare’s coverage is not unlimited. You will be responsible for a daily coinsurance amount after the 20th day of your stay, and Medicare will stop paying once you reach the 100-day limit. If you still need rehab after that point, you will need to pay for it out of pocket or through another insurance plan.
Q: What happens if I don’t meet Medicare’s requirements for rehab coverage?
A: If you don’t meet Medicare’s requirements for inpatient rehab coverage, you may still have other options. For example, you may be able to receive outpatient rehab services, which can include physical therapy, occupational therapy, and speech therapy. These services are typically less intensive than inpatient rehab, but they can still be very effective.
In addition, you may be able to get help from other sources, such as your state’s Medicaid program or a private insurance plan. Some rehab facilities also offer payment plans or sliding scale fees based on your income. It’s important to explore all of your options and talk to your healthcare providers about what’s best for you.
Q: Can I switch from inpatient rehab to outpatient rehab if I’m not making progress?
A: Yes, you can switch from inpatient rehab to outpatient rehab if you’re not making progress or if you no longer meet Medicare’s requirements for inpatient rehab. However, it’s important to work with your healthcare providers to determine the best course of action for your specific needs.
Keep in mind that switching to outpatient rehab may mean that you have to travel to a different facility or receive care on a different schedule. You may also need to pay for some or all of the costs out of pocket, depending on your insurance coverage. Be sure to discuss all of these factors with your healthcare providers before making a decision.
Q: What types of rehab services does Medicare cover?
A: Medicare covers a wide range of rehab services, including physical therapy, occupational therapy, and speech therapy. These services are designed to help you regain strength, mobility, and independence after an illness, injury, or surgery.
In addition, Medicare may cover other types of rehab services, such as cardiac rehab, pulmonary rehab, and substance abuse treatment. However, the specific services that are covered may vary depending on your individual needs and the policies of your healthcare providers.
Q: How do I know if I’m eligible for Medicare rehab coverage?
A: To be eligible for Medicare rehab coverage, you must be enrolled in Medicare Part A and you must meet certain requirements. These requirements include being hospitalized for at least three consecutive days, needing daily skilled care, and making progress towards your goals.
Your healthcare providers will work with you to determine whether you meet these requirements and what types of rehab services are appropriate for your needs. It’s also important to check with your insurance provider to understand your specific coverage and any out-of-pocket costs you may be responsible for.
In conclusion, Medicare can be a helpful resource for those seeking rehabilitation services. However, it’s important to understand the limitations and coverage restrictions associated with the program. While there is no set limit on how long Medicare will pay for rehab, coverage is typically based on medical necessity and progress towards recovery goals.
It’s important to keep in mind that Medicare coverage for rehab may differ depending on the specific plan and type of care needed. Patients should work closely with their healthcare providers and insurance companies to determine the best course of action for their individual needs.
Overall, Medicare can be a valuable resource for those seeking rehabilitation services. While coverage may be limited, it can help to offset the cost of care and provide a path towards recovery. By understanding the coverage limitations and working closely with healthcare providers, patients can make informed decisions about their rehab options.
Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior insurance, encompassing Medicare, Medigap, long-term care insurance, life insurance, and dental, vision, and hearing insurance. Vincent's unwavering passion for guiding seniors through the intricate insurance landscape and crafting customized solutions to address their individual needs has earned Over65InsuranceOptions an esteemed reputation as a dependable ally for seniors nationwide.
More Posts

