Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior...Read more
Medicare coverage is a crucial factor for many seniors who require rehabilitation services. However, the duration of Medicare coverage for rehabilitation can be confusing and overwhelming. How long does Medicare cover rehabilitation, and what are the criteria for receiving this coverage? In this article, we will explore the ins and outs of Medicare coverage for rehabilitation, giving you a better understanding of what to expect and how to plan for your rehabilitation needs. So, let’s dive in and explore this critical topic in-depth.
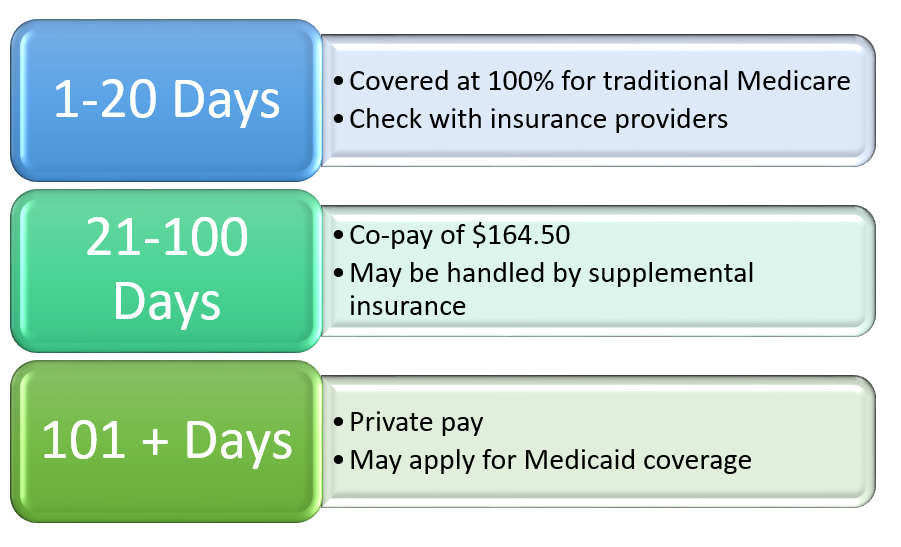
Medicare covers rehabilitation services for a limited time period. If you need rehabilitation services after an injury or illness, Medicare will cover up to 100 days of care in a skilled nursing facility. However, the first 20 days are fully covered, and for the next 80 days, you will need to pay a daily coinsurance fee. Medicare also covers rehabilitation services in other settings, such as outpatient clinics, but the duration of coverage may vary depending on your specific needs and conditions.
How Long Does Medicare Cover Rehabilitation?
Medicare is a federal health insurance program that covers eligible individuals who are 65 years or older, those with certain disabilities, and those with end-stage renal disease. One of the benefits of Medicare is coverage for rehabilitation services. Rehabilitation services are critical in helping individuals regain their independence and mobility after an injury, illness, or surgery. However, many people are unsure about how long Medicare covers rehabilitation services. In this article, we will explore the different types of rehabilitation services that Medicare covers and the duration of coverage.
Inpatient Rehabilitation Facility (IRF) Services
Inpatient rehabilitation facility (IRF) services are covered under Medicare Part A. IRFs are specialized facilities that provide intensive rehabilitation for patients who require a minimum of three hours of therapy per day. Medicare covers up to 90 days of inpatient rehabilitation per benefit period. If necessary, an additional 60 days of rehabilitation can be covered with a lifetime reserve day. During this time, Medicare covers 100% of the cost for the first 20 days. For days 21-100, Medicare covers all but a daily coinsurance amount.
If a patient requires additional rehabilitation beyond 100 days, they may be responsible for the full cost of the services. Alternatively, they may be able to receive outpatient rehabilitation services, which are covered under Medicare Part B.
Home Health Rehabilitation Services
Home health rehabilitation services are covered under Medicare Part A and Part B. These services are provided to patients who are homebound and require skilled nursing care or therapy services. Medicare covers home health rehabilitation services for as long as the patient requires them, as long as the services are medically necessary.
The frequency and duration of home health rehabilitation services are determined by the patient’s individual needs and treatment plan. Patients must have a doctor’s order for home health services, and the services must be provided by a Medicare-certified home health agency.
Outpatient Rehabilitation Services
Outpatient rehabilitation services are covered under Medicare Part B. These services are provided to patients who do not require hospitalization and can receive therapy services in an outpatient setting. Medicare covers a wide range of outpatient rehabilitation services, including physical therapy, occupational therapy, and speech-language pathology services.
Medicare covers outpatient rehabilitation services for as long as they are medically necessary. The frequency and duration of services are determined by the patient’s individual needs and treatment plan. Patients must have a doctor’s order for outpatient rehabilitation services, and the services must be provided by a Medicare-certified outpatient rehabilitation facility.
Benefits of Medicare Rehabilitation Coverage
Medicare rehabilitation coverage provides many benefits to eligible individuals. Rehabilitation services can help patients regain their independence, improve their quality of life, and reduce the risk of complications. Rehabilitation services can also help patients avoid hospital readmissions, which can be costly and disruptive.
Additionally, Medicare rehabilitation coverage can help patients save money on healthcare costs. Medicare covers a significant portion of the cost for rehabilitation services, which can be expensive. By having Medicare coverage, patients can receive the care they need without worrying about the financial burden.
Conclusion: Medicare Rehabilitation Coverage
Medicare provides coverage for rehabilitation services for eligible individuals. The duration of coverage depends on the type of rehabilitation services needed and the patient’s individual needs. Inpatient rehabilitation services are covered for up to 90 days per benefit period, with the possibility of an additional 60 days. Home health rehabilitation services are covered for as long as they are medically necessary, and outpatient rehabilitation services are covered for as long as they are medically necessary.
By having Medicare rehabilitation coverage, patients can receive the care they need to regain their independence, improve their quality of life, and reduce the risk of complications. Medicare rehabilitation coverage provides many benefits to eligible individuals, including cost savings and improved health outcomes.
Contents
Frequently Asked Questions
How long does Medicare cover rehabilitation?
Medicare coverage for rehabilitation services varies depending on the specific type of service being provided. In general, Medicare Part A covers inpatient rehabilitation in a hospital or skilled nursing facility for up to 100 days. After the first 20 days, there is a daily coinsurance cost that the patient is responsible for.
For outpatient rehabilitation services, Medicare Part B covers physical therapy, occupational therapy, and speech therapy. There is no limit on the amount of outpatient therapy services that Medicare will cover. However, there may be limitations on how many sessions a patient can receive per day or per week.
What types of rehabilitation services does Medicare cover?
Medicare covers a variety of rehabilitation services, including physical therapy, occupational therapy, and speech therapy. These services can be provided in different settings, such as inpatient hospitals, skilled nursing facilities, or outpatient clinics. Medicare also covers cardiac rehabilitation programs for patients with heart conditions, as well as pulmonary rehabilitation programs for patients with lung conditions.
In addition to traditional rehabilitation services, Medicare also covers “maintenance therapy” for patients with chronic conditions, such as Parkinson’s disease or multiple sclerosis. Maintenance therapy is designed to help patients maintain their current level of function and prevent further decline.
Do I need a referral for rehabilitation services?
In most cases, patients do not need a referral from their primary care physician to receive rehabilitation services under Medicare. However, there may be some exceptions depending on the specific type of service and the setting in which it is provided. For example, patients may need a referral for outpatient therapy services if they are receiving them from a private practice rather than a hospital or clinic.
It is always a good idea to check with your healthcare provider or Medicare to determine if a referral is necessary before seeking rehabilitation services.
Can I receive rehabilitation services at home?
Yes, Medicare covers home health services, which can include rehabilitation services provided in the patient’s home. To qualify for home health services, patients must be homebound and require skilled care, such as physical therapy or occupational therapy. Home health services are typically covered under Medicare Part A and may require a copayment.
Patients can also receive outpatient therapy services in their home if they are unable to leave their home due to a medical condition. However, these services may not be covered under Medicare and may require out-of-pocket payment.
What should I do if my Medicare coverage for rehabilitation services runs out?
If your Medicare coverage for rehabilitation services runs out, you may need to consider other options for continuing your care. Depending on your situation, you may be able to receive rehabilitation services through a private insurance plan, Medicaid, or through community-based programs.
It is important to discuss your options with your healthcare provider and insurance provider to determine the best course of action for continuing your rehabilitation care. You may also be eligible for financial assistance or other programs to help cover the cost of your care.
In conclusion, Medicare coverage for rehabilitation services varies depending on the type of service and the individual’s needs. While some services may be covered for a limited time, others may be covered for an extended period. It is important to understand the limitations and requirements of Medicare coverage for rehabilitation to ensure you receive the care you need.
If you or a loved one requires rehabilitation services, it is important to discuss your options with a healthcare professional to determine the best course of action. They can help you navigate the complex system of Medicare coverage and ensure you receive the care you need to achieve your health goals.
In summary, while Medicare coverage for rehabilitation may not be unlimited, it can still provide valuable support to those in need. By understanding the coverage limitations and working with healthcare professionals to develop a personalized care plan, you can receive the best possible care and improve your overall health and well-being.
Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior insurance, encompassing Medicare, Medigap, long-term care insurance, life insurance, and dental, vision, and hearing insurance. Vincent's unwavering passion for guiding seniors through the intricate insurance landscape and crafting customized solutions to address their individual needs has earned Over65InsuranceOptions an esteemed reputation as a dependable ally for seniors nationwide.
More Posts

