Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior...Read more
As we age, our bodies may experience certain conditions that require special medical attention. Incontinence is one such condition that affects many seniors. It can be an embarrassing and uncomfortable problem that can impact their daily lives. However, there is good news! Medicare may cover incontinence supplies for those who need them.
In this article, we’ll delve into the details of what Medicare covers when it comes to incontinence supplies. We’ll explore the different types of supplies available and what you need to do to qualify for coverage. So, if you or a loved one is struggling with incontinence, read on to find out how Medicare can help.
Yes, Medicare Part B may cover incontinence supplies such as catheters, external urinary collection devices, and certain adult diapers or pads if they are deemed medically necessary by a doctor. However, there are certain limitations and requirements that must be met for coverage. It is important to check with Medicare and your healthcare provider for more information.
Does Medicare Cover Incontinence Supplies?
Incontinence is a common condition among seniors, and it can have a significant impact on their quality of life. Many seniors require incontinence supplies, such as adult diapers, pads, and liners, to manage their symptoms. However, these supplies can be expensive, and many seniors rely on Medicare to help cover the costs. So, does Medicare cover incontinence supplies? Let’s explore the answer to this question in more detail.
Understanding Incontinence Supplies
Incontinence supplies are products that are designed to help manage the symptoms of urinary or fecal incontinence. These supplies can include adult diapers, pads, liners, and other products that are designed to absorb urine or fecal matter and prevent leaks. Incontinence supplies are not typically covered by traditional Medicare, but there are some situations where Medicare may provide coverage.
If you have a medical condition that causes incontinence, such as Parkinson’s disease, multiple sclerosis, or spinal cord injuries, you may be eligible for coverage of incontinence supplies under Medicare. In these cases, your doctor will need to provide documentation of your condition and the medical necessity of the supplies.
Medicare Coverage for Incontinence Supplies
If you are eligible for Medicare coverage of incontinence supplies, you will typically need to have a Medicare Advantage plan or a Medicare Supplement plan to receive coverage. Traditional Medicare does not cover these supplies, so you will need to enroll in a plan that offers this coverage.
Under Medicare Advantage plans, incontinence supplies may be covered as a supplemental benefit. However, the coverage offered by these plans can vary widely, so it’s important to read the fine print and understand your plan’s coverage limitations and requirements.
Medicare Supplement plans may also offer coverage for incontinence supplies, but again, the coverage offered can vary by plan. Some plans may cover a portion of the cost of the supplies, while others may provide full coverage.
Benefits of Medicare Coverage for Incontinence Supplies
If you are eligible for Medicare coverage of incontinence supplies, there are several benefits to consider. First, Medicare coverage can help reduce the out-of-pocket costs associated with these supplies, which can be significant. Second, having access to incontinence supplies can help improve your quality of life and make it easier to manage your symptoms.
In addition, Medicare coverage can help ensure that you have access to high-quality incontinence supplies that are designed to meet your specific needs. This can be especially important if you have a medical condition that requires specialized care.
Incontinence Supplies vs. Other Options
If you are not eligible for Medicare coverage of incontinence supplies, there are other options to consider. One option is to purchase these supplies out-of-pocket. While this can be expensive, it may be necessary if you cannot afford to enroll in a Medicare Advantage or Supplement plan.
Another option is to explore alternative treatments for incontinence, such as pelvic floor exercises, bladder training, or medication. These treatments can help improve your symptoms and reduce your reliance on incontinence supplies.
Conclusion
In summary, Medicare does not typically cover incontinence supplies under traditional Medicare. However, if you have a medical condition that causes incontinence, you may be eligible for coverage under a Medicare Advantage or Supplement plan. If you are not eligible for coverage, there are other options to consider, such as purchasing supplies out-of-pocket or exploring alternative treatments. Ultimately, the best course of action will depend on your specific needs and circumstances, so it’s important to talk to your doctor and explore all of your options.
Contents
- Frequently Asked Questions
- Does Medicare Cover Incontinence Supplies?
- How Do I Get Medicare Coverage for Incontinence Supplies?
- What If I Need Incontinence Supplies That Are Not Covered by Medicare?
- Are There Any Other Requirements for Medicare Coverage of Incontinence Supplies?
- Can I Get Incontinence Supplies Through Medicare Advantage?
- Are Catheter, Ostomy, and Incontinence Supplies Covered by Insurance? 180 Medical Explains.
Frequently Asked Questions
Does Medicare Cover Incontinence Supplies?
Yes, Medicare Part B may cover certain incontinence supplies, such as catheters, external urinary collection devices, and bags. However, Medicare does not cover adult diapers or other disposable incontinence products.
It’s important to note that in order for Medicare to cover incontinence supplies, they must be deemed medically necessary by a doctor. Additionally, there may be limitations on the quantity or frequency of supplies that are covered.
How Do I Get Medicare Coverage for Incontinence Supplies?
To get Medicare coverage for incontinence supplies, you will need a prescription from your doctor stating that the supplies are medically necessary. You will also need to purchase the supplies from a Medicare-approved supplier that accepts assignment.
It’s important to note that not all Medicare suppliers offer incontinence supplies, so you may need to do some research to find a supplier that does.
What If I Need Incontinence Supplies That Are Not Covered by Medicare?
If you need incontinence supplies that are not covered by Medicare, you may be able to get financial assistance through state programs or non-profit organizations. You can also shop around for lower-cost supplies or consider using reusable products to save money.
It’s important to talk to your doctor about all of your options for managing incontinence and to consider the potential costs and benefits of each.
Are There Any Other Requirements for Medicare Coverage of Incontinence Supplies?
In addition to needing a prescription and purchasing supplies from a Medicare-approved supplier, there may be other requirements for Medicare coverage of incontinence supplies. For example, you may need to have a certain type of incontinence or meet other medical criteria.
It’s important to talk to your doctor and your Medicare supplier to ensure that you meet all of the necessary requirements for coverage.
Can I Get Incontinence Supplies Through Medicare Advantage?
Yes, if you have a Medicare Advantage plan, you may be able to get coverage for incontinence supplies. However, the specific coverage and requirements may vary depending on your plan.
It’s important to review your plan’s benefits and speak with your doctor and Medicare Advantage plan provider to understand your coverage options and any potential out-of-pocket costs.
Are Catheter, Ostomy, and Incontinence Supplies Covered by Insurance? 180 Medical Explains.
In conclusion, Medicare does cover incontinence supplies, but there are certain requirements that must be met. Patients must have a doctor’s prescription for the supplies and they must be deemed medically necessary. Additionally, Medicare may only cover a portion of the cost, leaving the patient responsible for the remaining balance.
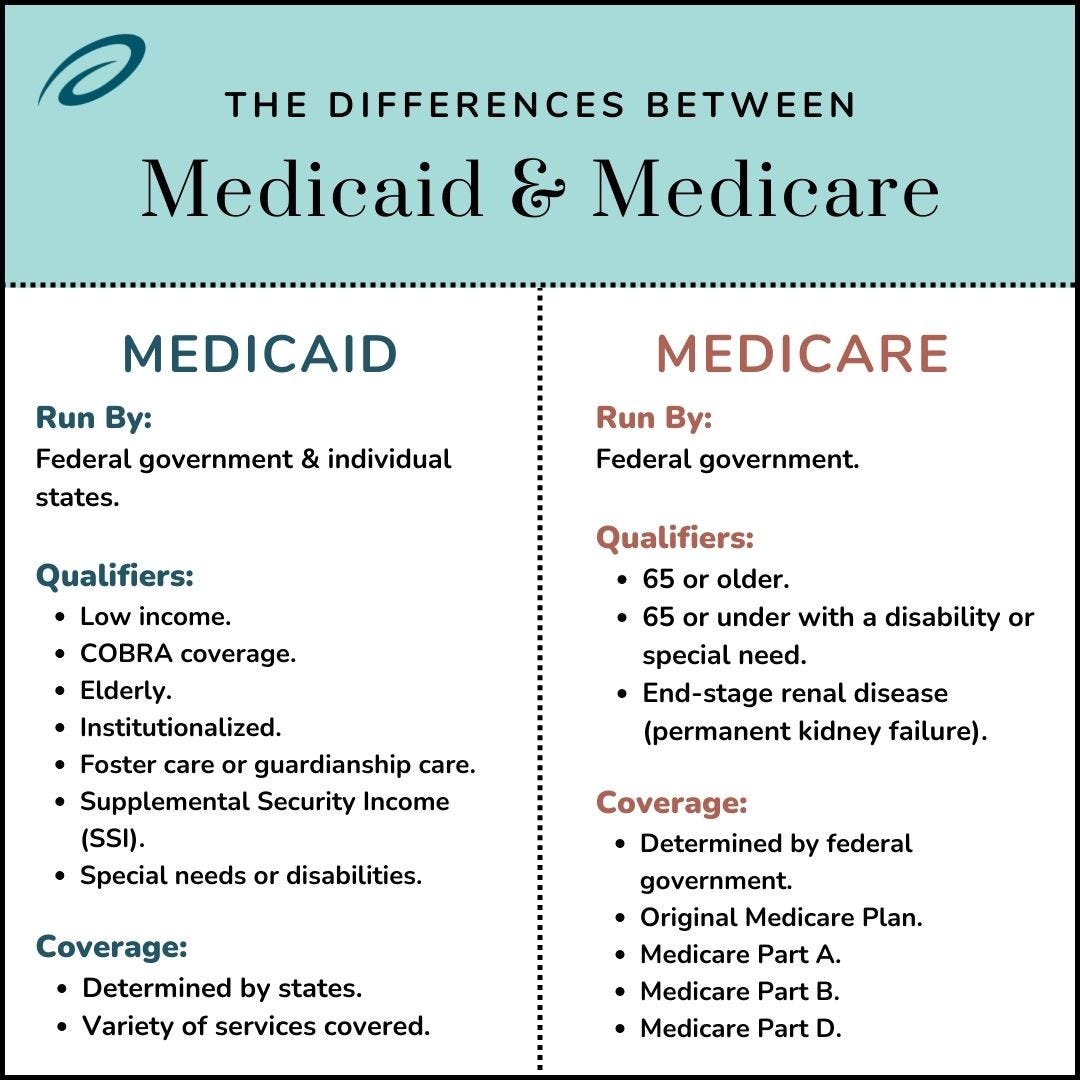
It is important for patients to be informed about their coverage options and to understand the limitations of their Medicare plan. Patients may also want to explore alternative coverage options, such as Medicaid or private insurance, to ensure they have access to the supplies they need.
Overall, while Medicare does provide coverage for incontinence supplies, patients should be aware of the specific requirements and potential out-of-pocket costs. By staying informed and exploring all available options, patients can ensure they receive the best possible care for their incontinence needs.
Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior insurance, encompassing Medicare, Medigap, long-term care insurance, life insurance, and dental, vision, and hearing insurance. Vincent's unwavering passion for guiding seniors through the intricate insurance landscape and crafting customized solutions to address their individual needs has earned Over65InsuranceOptions an esteemed reputation as a dependable ally for seniors nationwide.
More Posts

