Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior...Read more
As we age, our bodies become more vulnerable to various health issues that may require rehabilitation. Luckily, Medicare covers rehabilitation services to help seniors regain their strength and independence. However, understanding how long Medicare will pay for these services can be confusing.
The length of time Medicare covers rehabilitation depends on various factors such as the type of rehabilitation needed, the severity of the condition, and the progress made during the treatment. In this article, we will explore the different types of rehabilitation services covered by Medicare and the duration of coverage for each.
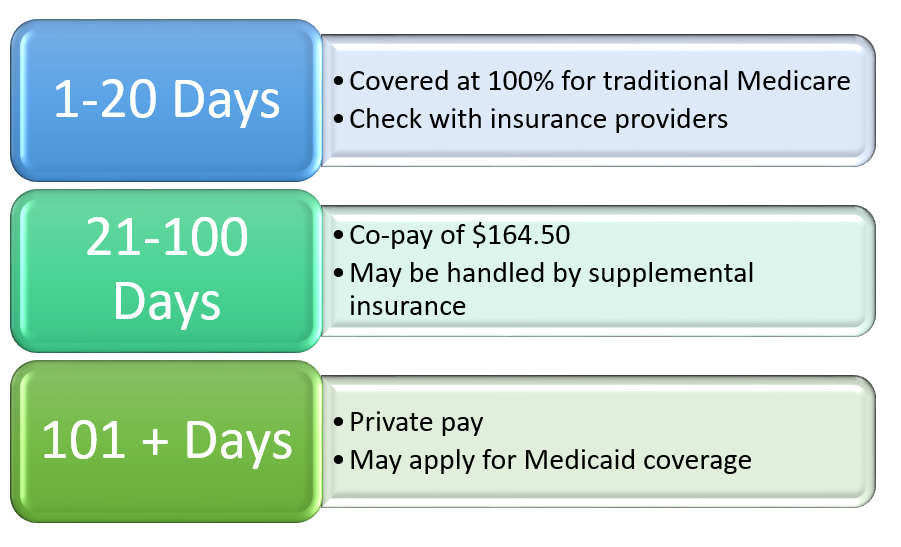
Medicare typically covers up to 100 days of rehabilitation care in a skilled nursing facility. The first 20 days are fully covered, and for days 21-100, a daily coinsurance fee may apply. However, Medicare will only pay for rehabilitation services that are deemed medically necessary and are provided by a Medicare-certified provider. It’s important to note that Medicare does not cover long-term care in a nursing facility.
How Long Does Medicare Pay for Rehabilitation?
When it comes to healthcare, Medicare is a crucial program that provides coverage for many Americans. This includes coverage for rehabilitation services, which can be essential for individuals recovering from an injury or illness. However, it is important to understand exactly how long Medicare will pay for rehabilitation services.
1. What is Rehabilitation?
Rehabilitation refers to a range of services designed to help individuals recover from an injury, illness, or surgery. These services can include physical therapy, occupational therapy, speech therapy, and more. Rehabilitation is often necessary to help individuals regain their strength, mobility, and independence.
When it comes to Medicare coverage for rehabilitation, it is important to understand that Medicare only covers medically necessary services. This means that the rehabilitation services must be deemed necessary by a healthcare provider in order to be covered.
2. Medicare Coverage for Inpatient Rehabilitation
For individuals who require inpatient rehabilitation, Medicare will cover the cost of care for up to 100 days per benefit period. This coverage includes all necessary services, such as room and board, nursing care, therapy services, and more.
It is important to note that Medicare will only cover inpatient rehabilitation if the individual requires daily therapy services and is making progress towards their recovery goals.
3. Medicare Coverage for Outpatient Rehabilitation
For individuals who require outpatient rehabilitation, Medicare will cover the cost of care as long as the services are deemed medically necessary. This can include services such as physical therapy, occupational therapy, and speech therapy.
However, it is important to understand that there may be certain limitations on Medicare coverage for outpatient rehabilitation. For example, there may be limits on the number of therapy sessions that are covered per year.
4. Medicare Coverage for Home Health Rehabilitation
For individuals who require rehabilitation services in the home, Medicare will cover the cost of care as long as the services are deemed medically necessary. This can include services such as physical therapy, occupational therapy, and speech therapy.
However, it is important to understand that there may be certain limitations on Medicare coverage for home health rehabilitation. For example, there may be limits on the number of therapy sessions that are covered per week.
5. Continuation of Medicare Coverage for Rehabilitation
In some cases, individuals may require rehabilitation services for an extended period of time. In these cases, Medicare may continue to cover the cost of care as long as the services are deemed medically necessary.
However, it is important to understand that Medicare will only continue to cover rehabilitation services if the individual is making progress towards their recovery goals.
6. Benefits of Medicare Coverage for Rehabilitation
One of the biggest benefits of Medicare coverage for rehabilitation is that it can help individuals recover from an injury or illness and regain their independence. Rehabilitation services can help individuals regain their strength, mobility, and ability to perform daily tasks.
In addition, Medicare coverage for rehabilitation can help individuals avoid costly healthcare expenses. Without coverage, rehabilitation services can be expensive and may be out of reach for many individuals.
7. Limitations of Medicare Coverage for Rehabilitation
While Medicare coverage for rehabilitation can be beneficial, it is important to understand that there may be certain limitations on coverage. For example, there may be limits on the number of therapy sessions that are covered per year or per week.
In addition, some rehabilitation services may not be covered by Medicare at all. It is important to check with your healthcare provider and your Medicare plan to understand exactly what services are covered.
8. Medicare Coverage for Rehabilitation vs. Private Insurance
When it comes to coverage for rehabilitation services, Medicare and private insurance plans may differ. Private insurance plans may offer more comprehensive coverage for rehabilitation services, but may also come with higher costs.
It is important to understand the specifics of your insurance plan and to compare coverage options when choosing a plan.
9. Conclusion
Medicare coverage for rehabilitation services can be essential for individuals recovering from an injury or illness. However, it is important to understand the limitations of coverage and to work with your healthcare provider to ensure that you receive the services you need.
If you have questions about Medicare coverage for rehabilitation services, be sure to speak with your healthcare provider and your Medicare plan to understand exactly what services are covered.
10. Table of Medicare Coverage for Rehabilitation
| Type of Rehabilitation | Medicare Coverage |
| — | — |
| Inpatient Rehabilitation | Up to 100 days per benefit period |
| Outpatient Rehabilitation | Covered as long as services are deemed medically necessary |
| Home Health Rehabilitation | Covered as long as services are deemed medically necessary |
| Continuation of Medicare Coverage | Covered as long as services are deemed medically necessary |
Overall, understanding Medicare coverage for rehabilitation services is important for individuals who may require these services. By understanding the specifics of coverage, individuals can ensure that they receive the care they need without facing excessive healthcare expenses.
Contents
Frequently Asked Questions
In this section, we will answer some of the most commonly asked questions about Medicare coverage for rehabilitation.
How long will Medicare pay for rehabilitation?
Medicare will pay for rehabilitation services as long as they are deemed medically necessary. The length of time can vary depending on the individual’s condition, progress, and treatment plan. Some people may only need a few weeks of rehab, while others may require months or even years of treatment. It is important to work with your healthcare team to determine the appropriate length of time for your rehabilitation.
It is also important to note that Medicare has a yearly limit on how much it will pay for therapy services. Once this limit is reached, you may have to pay out of pocket for additional services or seek alternative forms of treatment.
What types of rehabilitation services does Medicare cover?
Medicare covers a wide range of rehabilitation services, including physical therapy, occupational therapy, and speech therapy. These services are typically provided by licensed healthcare professionals and are aimed at helping individuals recover from an injury or illness, improve their mobility and strength, and regain their independence.
In addition to therapy services, Medicare also covers certain types of durable medical equipment (DME) that may be necessary for rehabilitation, such as wheelchairs, walkers, and hospital beds.
Do I need a referral from my doctor for rehabilitation services?
In most cases, yes. Medicare requires a referral from a healthcare provider in order to cover rehabilitation services. This referral must be from a doctor or other qualified healthcare professional and must be based on a specific diagnosis or medical condition. Your healthcare provider can help you determine if you need a referral for rehabilitation services.
It is also important to note that some rehabilitation services may require prior authorization from Medicare before they can be covered. Your healthcare provider can help you navigate this process and ensure that you receive the necessary care.
Can I receive rehabilitation services in my home?
Yes. Medicare covers certain types of rehabilitation services that can be provided in the home, such as physical therapy and occupational therapy. In order to qualify for home-based rehabilitation services, you must meet certain eligibility criteria and have a healthcare provider prescribe the services.
Home-based rehabilitation services can be a convenient and cost-effective option for individuals who have difficulty leaving their homes or who live in remote areas. However, it is important to note that not all types of rehabilitation services can be provided in the home, and the availability of home-based services may vary depending on your location and healthcare provider.
What should I do if my Medicare coverage for rehabilitation is denied?
If your Medicare coverage for rehabilitation services is denied, you have the right to appeal the decision. The appeals process allows you to challenge the denial and provide additional information or evidence to support your case.
To appeal a Medicare decision, you will need to follow a specific process and meet certain deadlines. Your healthcare provider or a Medicare representative can help you navigate this process and ensure that your rights are protected.
In conclusion, Medicare is a vital resource for individuals who require rehabilitation services. However, it is crucial to understand that there are limitations to Medicare coverage. The length of time that Medicare will pay for rehabilitation services depends on the individual’s specific needs and circumstances.
It is important to note that Medicare does not cover all rehabilitation services. For example, Medicare does not cover custodial care or long-term care in nursing homes. Additionally, Medicare may only cover a certain number of days for inpatient rehabilitation services.
To ensure that you receive the appropriate level of coverage, it is essential to work with your healthcare provider and Medicare to understand your specific needs and coverage options. By doing so, you can ensure that you receive the rehabilitation services you need to achieve your optimal health and wellbeing.
Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior insurance, encompassing Medicare, Medigap, long-term care insurance, life insurance, and dental, vision, and hearing insurance. Vincent's unwavering passion for guiding seniors through the intricate insurance landscape and crafting customized solutions to address their individual needs has earned Over65InsuranceOptions an esteemed reputation as a dependable ally for seniors nationwide.
More Posts

