Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior...Read more
Are you or someone you know considering therapy but don’t know what Medicare will cover? Well, you’re not alone. Many people are unsure about what mental health services are covered under Medicare. In this article, we will dive into the details of how many therapy sessions Medicare covers and what you need to know before making an appointment with a mental health professional. Whether you’re a senior citizen or someone with a disability, understanding your Medicare coverage for mental health services is crucial to getting the care you need.
Contents
- How Many Therapy Sessions Does Medicare Cover?
- Frequently Asked Questions
- What is Medicare coverage for therapy sessions?
- How many therapy sessions does Medicare cover?
- How do I find a mental health professional who accepts Medicare?
- Can I receive therapy sessions through telehealth or online services?
- What should I do if I have a complaint or concern about my therapy sessions?
- Will Medicare Cover My Procedure? What’s Covered by Medicare
How Many Therapy Sessions Does Medicare Cover?
If you or a loved one needs physical, occupational, or speech therapy, Medicare can help cover the costs. However, it’s important to understand how many therapy sessions Medicare covers and what types of therapy are eligible. Here’s a breakdown of what you need to know.
Types of Therapy Covered by Medicare
Medicare covers three main types of therapy: physical therapy, occupational therapy, and speech therapy. Physical therapy helps improve mobility and strength, while occupational therapy focuses on helping patients regain the ability to perform daily tasks. Speech therapy is designed to help patients with communication and swallowing disorders.
To be eligible for therapy coverage under Medicare, the therapy must be deemed “medically necessary.” This means that the therapy is needed to treat a specific condition or injury and must be prescribed by a healthcare provider.
Physical Therapy
Medicare covers physical therapy for a variety of conditions, including arthritis, joint replacements, and stroke. The number of therapy sessions covered by Medicare varies depending on the type of therapy and the patient’s needs. Generally, Medicare covers up to 80% of the cost of physical therapy sessions, and the patient is responsible for the remaining 20%.
For example, Medicare covers up to 100 sessions of physical therapy per year for patients with a chronic condition. Patients who require additional therapy may be eligible for more sessions if their healthcare provider deems it medically necessary.
Occupational Therapy
Occupational therapy helps patients regain the ability to perform daily tasks such as dressing, grooming, and cooking. Medicare covers up to 80% of the cost of occupational therapy sessions, and patients are responsible for the remaining 20%.
Patients with a chronic condition may be eligible for up to 100 sessions of occupational therapy per year. However, additional sessions may be covered if deemed medically necessary by a healthcare provider.
Speech Therapy
Medicare covers speech therapy for patients with communication and swallowing disorders. The number of therapy sessions covered by Medicare varies based on the patient’s needs and the type of therapy required.
Medicare covers up to 80% of the cost of speech therapy sessions, and patients are responsible for the remaining 20%. Patients with a chronic condition may be eligible for up to 100 sessions of speech therapy per year, and additional sessions may be covered if deemed medically necessary.
Benefits of Medicare Coverage for Therapy
One of the main benefits of Medicare coverage for therapy is that it can significantly reduce out-of-pocket costs for patients. This can be especially beneficial for patients who require multiple therapy sessions over an extended period of time.
In addition, Medicare coverage for therapy can help improve patients’ quality of life by helping them regain mobility, independence, and the ability to communicate effectively.
Out-of-Pocket Costs for Therapy
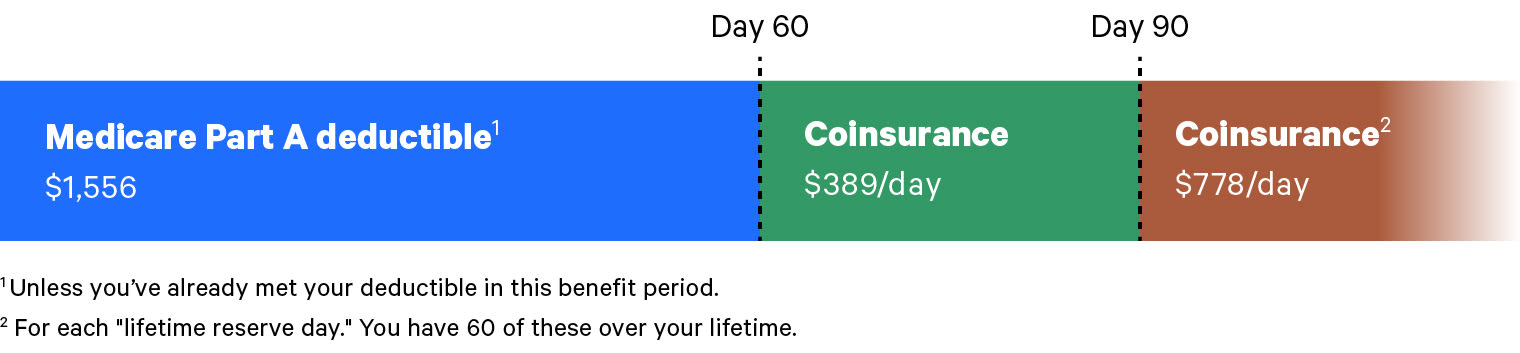
While Medicare covers a portion of the cost of therapy sessions, patients are responsible for the remaining 20% of the cost. Patients may also be responsible for deductibles and copayments, depending on their specific Medicare plan.
It’s important to talk to your healthcare provider and Medicare representative to understand your specific out-of-pocket costs for therapy. Some patients may be eligible for financial assistance to help cover these costs.
Therapy Vs. Skilled Nursing Facility Care
Medicare also covers skilled nursing facility care for patients who require long-term care after a hospitalization or surgery. However, it’s important to note that therapy services provided in a skilled nursing facility may be subject to different coverage rules and limitations than therapy services provided in an outpatient setting.
It’s important to talk to your healthcare provider and Medicare representative to understand your coverage options for both therapy and skilled nursing facility care.
Conclusion
Medicare can be a valuable resource for patients who require physical, occupational, or speech therapy. While the number of therapy sessions covered by Medicare varies based on the patient’s needs and the type of therapy required, Medicare coverage can significantly reduce out-of-pocket costs for patients and help improve their quality of life.
If you or a loved one requires therapy, it’s important to talk to your healthcare provider and Medicare representative to understand your coverage options and out-of-pocket costs.
Frequently Asked Questions
Medicare provides coverage for a variety of mental health services, including therapy sessions. However, many beneficiaries are unsure of how many sessions are covered by Medicare. Here are the answers to some frequently asked questions about Medicare coverage for therapy sessions.
What is Medicare coverage for therapy sessions?
Medicare provides coverage for therapy sessions that are medically necessary to treat a mental health condition. This includes individual and group therapy sessions with a licensed mental health professional such as a psychologist or clinical social worker. Medicare covers these sessions at 80% of the Medicare-approved amount, and the remaining 20% is typically covered by a secondary insurance or out-of-pocket by the beneficiary.
It is important to note that Medicare does not cover couples or family therapy sessions. Additionally, Medicare only covers therapy sessions that are provided in a mental health facility or office, and not through telehealth or online services.
How many therapy sessions does Medicare cover?
Medicare covers an unlimited number of therapy sessions that are medically necessary to treat a mental health condition. However, beneficiaries may be subject to certain limitations on the number of sessions they can receive in a given time period. For example, Medicare may limit the number of sessions to one per week or per month. The exact number of sessions covered by Medicare will depend on the individual’s specific mental health needs.
Beneficiaries should also be aware that Medicare requires a mental health treatment plan to be created by their provider in order to receive coverage for therapy sessions. The treatment plan must include the beneficiary’s diagnosis, treatment goals, and the specific services that will be provided to address their mental health condition.
How do I find a mental health professional who accepts Medicare?
Beneficiaries can use Medicare’s “Physician Compare” tool on Medicare.gov to search for mental health professionals who accept Medicare. They can also contact their local Medicare office or State Health Insurance Assistance Program (SHIP) for assistance in finding a provider. It is important to ensure that the provider is enrolled in Medicare and accepts Medicare assignment, which means they agree to accept the Medicare-approved amount as payment in full.
Beneficiaries should also check with their secondary insurance or Medigap plan to ensure that the provider is in their network and covered under their plan.
Can I receive therapy sessions through telehealth or online services?
Medicare does provide coverage for certain telehealth services, including therapy sessions, but there are certain limitations. Medicare only covers telehealth services that are provided through live video conferencing between the beneficiary and the provider. Audio-only or email therapy sessions are not covered by Medicare.
Additionally, telehealth services are subject to the same coverage rules and limitations as in-person therapy sessions. Beneficiaries must have a mental health treatment plan in place, and the services must be medically necessary to treat a mental health condition. The provider must also be enrolled in Medicare and accept Medicare assignment.
What should I do if I have a complaint or concern about my therapy sessions?
If a beneficiary has a complaint or concern about their therapy sessions, they should first try to resolve the issue with their mental health provider. If the issue cannot be resolved, they can contact their local Medicare office or State Health Insurance Assistance Program (SHIP) for assistance. Beneficiaries can also file a complaint with Medicare by calling 1-800-MEDICARE (1-800-633-4227) or by visiting Medicare.gov.
Additionally, beneficiaries can contact the National Alliance on Mental Illness (NAMI) Helpline at 1-800-950-NAMI (6264) for support and resources related to mental health care.
Will Medicare Cover My Procedure? What’s Covered by Medicare
In conclusion, Medicare provides coverage for therapy sessions, but the number of sessions covered can vary depending on the type of therapy and the individual’s needs. It is important to understand the limitations and requirements of Medicare coverage to ensure you receive the appropriate care.
While coverage may be limited, Medicare does provide resources to help individuals find therapists and treatment options that fit their needs. It is important to take advantage of these resources and work closely with your healthcare provider to determine the best course of treatment.
Ultimately, the number of therapy sessions covered by Medicare should not deter individuals from seeking the care they need. By staying informed and advocating for oneself, individuals can receive the necessary treatment to improve their mental health and overall well-being.
Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior insurance, encompassing Medicare, Medigap, long-term care insurance, life insurance, and dental, vision, and hearing insurance. Vincent's unwavering passion for guiding seniors through the intricate insurance landscape and crafting customized solutions to address their individual needs has earned Over65InsuranceOptions an esteemed reputation as a dependable ally for seniors nationwide.
More Posts