Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior...Read more
Medicare Supplement Insurance Plans are a popular choice among seniors who want additional coverage for their healthcare needs. However, not many people know who regulates these plans. In this article, we will explore the regulatory bodies that oversee Medicare Supplement Insurance Plans and what it means for consumers.
The federal government oversees the regulation of Medicare Supplement Insurance Plans, but each state may have its own rules and regulations. It’s essential to understand how these plans are regulated so that you can make informed decisions about your healthcare coverage. So, let’s dive in and learn more about who regulates Medicare Supplement Insurance Plans.
Contents
- Who Regulates Medicare Supplement Insurance Plans?
- Frequently Asked Questions
- 1. Who regulates Medicare Supplement Insurance Plans?
- 2. What is the role of the Centers for Medicare and Medicaid Services (CMS) in regulating Medicare Supplement Insurance Plans?
- 3. How do state insurance departments regulate Medicare Supplement Insurance Plans?
- 4. What are some consumer protections in place for Medicare Supplement Insurance Plans?
- 5. Can Medicare Advantage plans be considered Medicare Supplement Insurance Plans?
Who Regulates Medicare Supplement Insurance Plans?
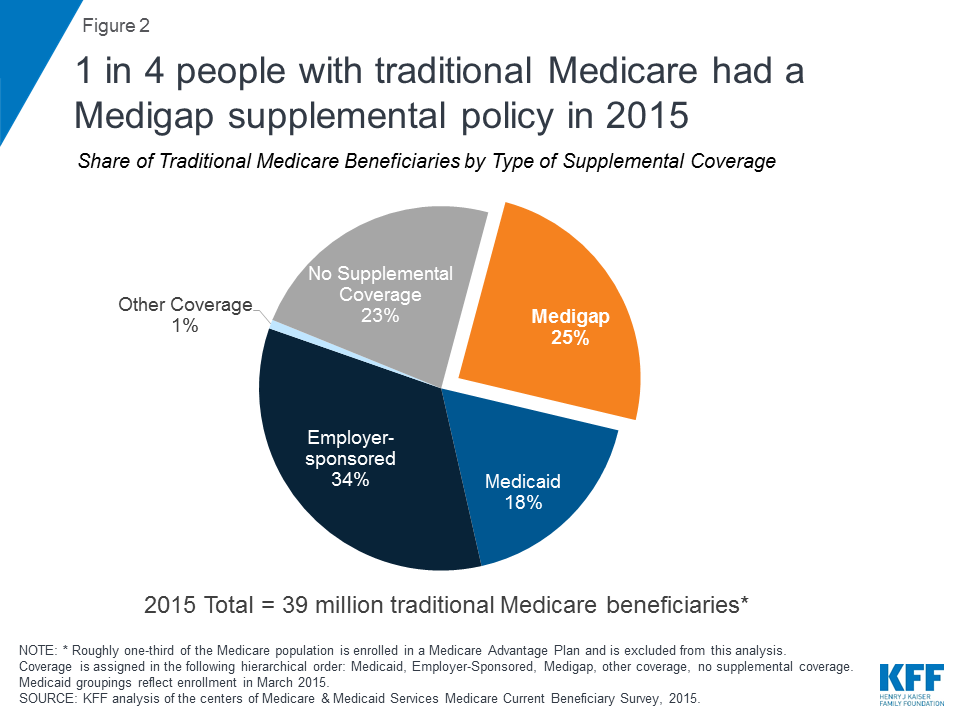
Medicare Supplement Insurance Plans, also known as Medigap, are private health insurance policies that help cover the costs of healthcare services that are not covered by Original Medicare. These plans are regulated by federal and state laws to ensure that insurance companies provide standardized benefits and follow specific guidelines. In this article, we’ll explore who regulates Medicare Supplement Insurance Plans, what their responsibilities are, and how they protect consumers.
Regulation by the Federal Government
The Centers for Medicare and Medicaid Services (CMS) is the federal agency responsible for overseeing Medicare Supplement Insurance Plans. They regulate the plans by setting standards for the benefits that must be offered, as well as the way the plans are marketed and sold. CMS also ensures that insurance companies follow federal laws and regulations, such as the Medicare Access and CHIP Reauthorization Act (MACRA).
One of the most important responsibilities of CMS is to review and approve the standardized Medigap plans. There are ten standardized plans, labeled A through N, and each plan offers a different set of benefits. Insurance companies are required to offer Plan A, but they can choose whether or not to offer the other plans. CMS ensures that all insurance companies that offer Medigap plans follow the same standard benefits for each plan.
Regulation by State Governments
In addition to federal regulation, each state has its own regulatory agency that oversees Medicare Supplement Insurance Plans. These agencies are responsible for enforcing state laws and regulations, as well as monitoring the financial stability of insurance companies that offer Medigap plans. They also provide consumer protection by investigating complaints and ensuring that insurance companies follow state guidelines for marketing and sales practices.
State regulatory agencies have the authority to approve or deny rate increases for Medigap plans. This means that insurance companies must submit their proposed rate increases to the state agency for approval before they can be implemented. The agency must review the rate increase to ensure that it is reasonable and not excessive. This helps protect consumers from paying too much for their Medigap coverage.
Benefits of Regulating Medicare Supplement Insurance Plans
Regulation of Medicare Supplement Insurance Plans provides several benefits for consumers. First, it ensures that insurance companies follow standardized benefits for each plan, which makes it easier for consumers to compare plans and choose the one that best fits their needs. Second, regulation helps protect consumers from fraudulent or deceptive marketing practices by requiring insurance companies to be transparent about the benefits and costs of their plans.
Third, regulation helps ensure that insurance companies are financially stable and able to pay claims. State regulatory agencies monitor the financial stability of insurance companies and can take action if they are not meeting financial requirements. This helps protect consumers from losing their coverage if an insurance company goes bankrupt.
Medicare Supplement Insurance Plans vs. Medicare Advantage Plans
It’s important to note that Medicare Supplement Insurance Plans are different from Medicare Advantage Plans. Medicare Advantage Plans are health insurance plans offered by private insurance companies that provide Medicare Part A and Part B benefits, as well as additional benefits such as prescription drug coverage, dental, vision, and hearing coverage. Medicare Advantage Plans are regulated by CMS and state agencies, but they have different rules and requirements than Medigap plans.
One key difference between the two types of plans is that Medicare Advantage Plans have networks of healthcare providers that patients must use in order to receive coverage. Medigap plans, on the other hand, allow patients to use any healthcare provider that accepts Medicare. Another difference is that Medicare Advantage Plans can have different costs for different services, while Medigap plans are standardized and have the same cost-sharing requirements for each plan.
Conclusion
In conclusion, Medicare Supplement Insurance Plans are regulated by both federal and state agencies to ensure that insurance companies offer standardized benefits and follow specific guidelines. This regulation provides several benefits for consumers, including transparency, financial stability, and protection from fraudulent marketing practices. It’s important to understand the differences between Medigap plans and Medicare Advantage Plans to choose the best coverage for your healthcare needs.
Frequently Asked Questions
1. Who regulates Medicare Supplement Insurance Plans?
Medicare Supplement Insurance Plans, also known as Medigap, are regulated by both the federal and state governments. The Centers for Medicare and Medicaid Services (CMS) is the federal agency responsible for overseeing Medicare, while each state has its own insurance department that regulates insurance companies operating within its borders.
Medigap plans must adhere to federal and state regulations, which include standardized benefit options, guaranteed renewable coverage, and protection against unfair marketing practices. In addition, states have the authority to set their own rules and requirements for Medigap policies, such as pricing standards and consumer protections.
2. What is the role of the Centers for Medicare and Medicaid Services (CMS) in regulating Medicare Supplement Insurance Plans?
The Centers for Medicare and Medicaid Services (CMS) is the federal agency responsible for overseeing Medicare and, as such, has a role in regulating Medicare Supplement Insurance Plans. CMS is responsible for setting the standardized benefit options for Medigap plans, which include ten different coverage options labeled A through N.
CMS also sets rules and guidelines for insurance companies offering Medigap policies, such as requirements for guaranteed renewable coverage and protections against discriminatory practices based on health status. In addition, CMS provides educational resources and information for consumers on Medigap plans and their coverage options.
3. How do state insurance departments regulate Medicare Supplement Insurance Plans?
Each state has its own insurance department that regulates insurance companies operating within its borders, including those offering Medicare Supplement Insurance Plans. State insurance departments set rules and requirements for insurers offering Medigap policies, such as pricing standards and consumer protections.
In addition, state insurance departments are responsible for overseeing the sale and marketing of Medigap policies within their states to ensure that insurers are not engaging in unfair or deceptive practices. Consumers can contact their state insurance department for information on Medigap policies, pricing, and consumer protections specific to their state.
4. What are some consumer protections in place for Medicare Supplement Insurance Plans?
Medicare Supplement Insurance Plans are required to adhere to federal and state regulations that provide consumer protections. For example, Medigap policies must be guaranteed renewable, meaning that insurers cannot cancel a policy as long as premiums are paid on time.
In addition, Medigap policies must cover certain benefits, depending on the plan type, such as Part A and Part B coinsurance and deductibles. Insurers are also prohibited from discriminating against applicants based on health status or charging higher premiums based on pre-existing conditions. Consumers can contact their state insurance department for information on additional consumer protections specific to their state.
5. Can Medicare Advantage plans be considered Medicare Supplement Insurance Plans?
No, Medicare Advantage plans are not considered Medicare Supplement Insurance Plans. Medicare Advantage plans are an alternative way to receive Medicare benefits, while Medigap policies are designed to supplement Original Medicare (Parts A and B).
Medicare Advantage plans are offered by private insurance companies and generally provide all of the Part A and Part B benefits, as well as additional benefits such as prescription drug coverage. Medigap policies, on the other hand, are designed to fill in the “gaps” in coverage left by Original Medicare, such as deductibles and coinsurance.
In conclusion, understanding who regulates Medicare supplement insurance plans is crucial for anyone seeking additional coverage beyond what Medicare provides. While Medicare itself is regulated by the federal government, the regulation of Medigap plans varies by state. This means that the rules and requirements for Medigap plans may differ depending on where you live.
Despite this variability, it is important to note that all Medigap plans must adhere to certain federal guidelines in order to provide coverage. These guidelines ensure that consumers are protected from unfair practices and receive the benefits they are promised.
Overall, it is important to do your research and carefully consider your options when selecting a Medicare supplement insurance plan. By understanding who regulates these plans and what guidelines they must follow, you can make an informed decision and find the coverage that best meets your needs.
Vincent Thrasher, the pioneering founder of Over65InsuranceOptions, has an impressive 20-year tenure in the insurance industry. His in-depth expertise spans the entire spectrum of senior insurance, encompassing Medicare, Medigap, long-term care insurance, life insurance, and dental, vision, and hearing insurance. Vincent's unwavering passion for guiding seniors through the intricate insurance landscape and crafting customized solutions to address their individual needs has earned Over65InsuranceOptions an esteemed reputation as a dependable ally for seniors nationwide.
More Posts

